Common Findings in Brain Imaging for Headaches
Structural Abnormalities
When investigating headaches, brain imaging techniques like MRI and CT scans often uncover structural irregularities. These can include harmless variations in brain anatomy or more concerning issues such as tumors, cysts, or arteriovenous malformations (AVMs). Spotting these structural differences is vital for distinguishing between ordinary headaches and those caused by serious underlying conditions. Early identification allows for prompt treatment and better symptom management.
Vascular Findings
Headaches frequently stem from vascular irregularities in the brain. Imaging can detect problems like narrowed or enlarged blood vessels, or the presence of aneurysms. These vascular issues may compress nearby tissues, causing pain and sometimes additional neurological symptoms. Inflammation or damage to blood vessels, visible on scans, can also trigger headache episodes.
Hydrocephalus
Excessive cerebrospinal fluid (CSF) accumulation, known as hydrocephalus, often causes headaches among other symptoms. Brain imaging clearly shows enlarged ventricles due to CSF buildup. Determining the severity and location of fluid retention is crucial for treatment planning, which may involve surgery to relieve pressure on the brain.
Inflammatory Processes
Brain inflammation from infections or autoimmune disorders can lead to headaches. MRI scans effectively reveal signs of inflammation like swelling or edema. These inflammatory responses may increase intracranial pressure, intensifying headache pain. Accurate detection of inflammation markers guides treatment toward addressing the root cause.
Degenerative Changes
Aging often brings degenerative brain changes that may contribute to headaches. Imaging can show tissue shrinkage (atrophy) associated with conditions like Alzheimer's disease. Assessing these changes helps determine their potential impact on headache patterns and overall brain function.
Metabolic Abnormalities
Some metabolic disorders affect brain function and cause headaches. While imaging doesn't directly show metabolic issues, it can reveal indirect indicators like altered brain metabolism or blood flow patterns. These imaging clues help identify metabolic causes and direct appropriate diagnostic testing and treatment.
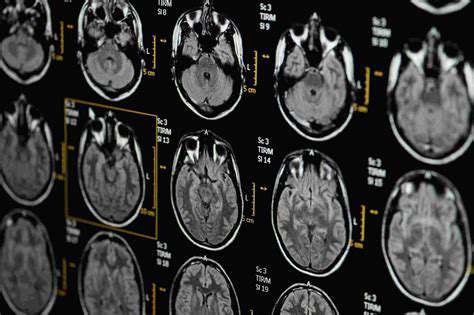
Analyzing MRI Scans for Headaches
Pre-Scan Considerations and Patient Preparation
Proper preparation is essential for successful MRI scans to evaluate headaches. Patients must disclose any metallic implants, devices, or prior surgeries that could affect the scan. Following pre-scan guidelines regarding medications, fasting, and clothing helps ensure optimal imaging quality. This preparation minimizes complications and facilitates accurate diagnosis.
MRI Scan Techniques and Image Acquisition
Different MRI techniques target specific aspects of brain structure and function relevant to headaches. Advanced sequences like diffusion-weighted imaging (DWI) detect water diffusion abnormalities indicating stroke or inflammation. Perfusion-weighted imaging (PWI) evaluates blood flow, identifying areas with reduced circulation that might trigger headaches. Using these specialized techniques provides comprehensive data for thorough evaluation.
Interpretation of MRI Findings Related to Headaches
Expert radiologists carefully analyze MRI results to identify headache-related abnormalities like tumors or vascular malformations. This detailed assessment differentiates between benign and serious causes. Interpretation incorporates the patient's medical history and symptoms for accurate diagnosis and treatment planning.
Correlation with Clinical Symptoms and Diagnosis
Linking MRI findings to the patient's symptoms is crucial for accurate diagnosis. For example, matching tumor location with headache patterns strengthens diagnostic confidence. This comprehensive approach ensures precise diagnosis and appropriate treatment strategies.
Potential Headaches Related to Brain Pathology
MRI scans reveal various headache-causing pathologies including tumors, aneurysms, and infections. Identifying these conditions is essential for proper treatment and management. Understanding how observed abnormalities relate to symptoms guides effective intervention.
The Role of Clinical Context in Interpretation
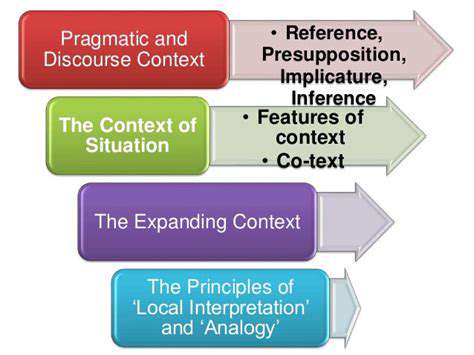
Clinical Context and Diagnostic Accuracy
A patient's complete clinical picture is essential for accurate diagnosis. Context helps distinguish between similar symptoms and identify their true cause. For instance, evaluating a cough differs significantly between asthma patients and healthy individuals.
Patient History and Symptom Evaluation
Detailed patient history including medical background, medications, and symptom characteristics is vital. Documenting symptom onset, duration, and associated features enables precise assessment.
Physical Examination and Findings
Physical exam results complement patient history. Findings like vital signs and skin changes, interpreted in context, help narrow diagnostic possibilities. For example, rash with fever suggests specific infections.
Laboratory and Imaging Results
Test results must align with clinical context. Abnormal findings require correlation with other data for accurate interpretation. Imaging and lab tests confirm or rule out suspected diagnoses.
Differential Diagnosis and Hypothesis Generation
Considering multiple potential diagnoses is crucial. Developing and testing hypotheses based on clinical context refines the diagnostic process.
Treatment Planning and Monitoring
Effective treatment plans account for individual patient needs and context. Regular monitoring ensures treatment efficacy and allows for adjustments.
Ethical Considerations and Patient Preferences
Respecting patient autonomy and values is paramount. Understanding patient perspectives ensures treatment aligns with their wishes and improves outcomes.