Targeting Neuroinflammation Beyond CGRP
Chronic pain frequently involves intricate inflammatory processes that extend far beyond the initial injury site. While CGRP inhibitors have demonstrated potential, addressing the root causes of neuroinflammation presents a substantial opportunity for developing more comprehensive and effective pain management approaches. Understanding and modulating the inflammatory cascade within the nervous system proves essential for achieving lasting pain relief and enhancing patient outcomes.
Modulating Microglial Activity
The central nervous system's resident immune cells, microglia, play a pivotal role in both initiating and perpetuating chronic pain states. When microglial activity becomes dysregulated, it can lead to persistent inflammation and neuronal damage. Developing therapies that specifically regulate microglial activation while preserving their vital functions represents a crucial advancement in innovative pain management strategies.
Interfering with Neuronal Excitability
Mechanisms controlling neuronal excitability significantly contribute to chronic pain conditions. Excessive neuronal firing, commonly associated with hyperalgesia and allodynia, can create a self-perpetuating cycle of pain amplification. Targeting the molecular pathways responsible for altered neuronal excitability offers a promising approach to pain relief by diminishing both the intensity and frequency of pain signals.
Blocking Nociceptive Transmission
Nociceptive transmission - the process converting harmful stimuli into pain signals - constitutes a fundamental element in chronic pain. Disrupting this transmission at various points along the pathway, from peripheral to central nervous systems, could yield novel therapeutic opportunities. This might involve targeting specific receptors or channels participating in the transmission process.
Modulating Endogenous Opioid Systems
The body's natural opioid system plays an indispensable role in pain modulation. When this system becomes dysregulated, it can contribute to chronic pain conditions. Therapies that enhance or modulate endogenous opioid system activity could provide a powerful strategy for pain management, potentially leading to more sustained and effective relief.
Addressing Peripheral Nerve Damage
Peripheral nerve damage represents a significant factor in numerous chronic pain conditions, often leading to altered nerve function and heightened pain sensitivity. Developing treatments focused on nerve repair or regeneration, or mitigating nerve injury effects, shows considerable promise. This approach might utilize growth factors, neurotrophic factors, or other molecules that promote nerve healing.
Promoting Neuroprotective Mechanisms
Chronic pain frequently involves neuronal damage and loss. Supporting neuroprotective mechanisms could offer a strategy for preserving nervous system integrity and reducing long-term pain consequences. Approaches that enhance neuronal survival, decrease oxidative stress, and facilitate neuronal repair represent promising directions for developing effective, long-term pain management solutions.
Peptide Delivery Systems: Enhancing Efficacy and Safety
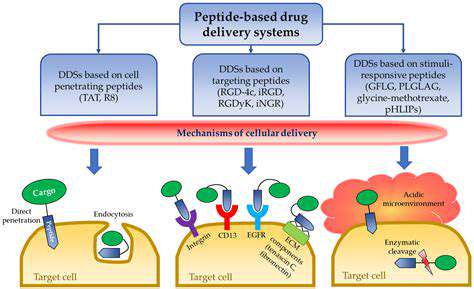
Targeted Delivery
Peptide delivery systems prove essential for optimizing therapeutic peptide efficacy and safety. A critical feature involves the capacity to direct peptides to specific cells or tissues. This targeted approach minimizes off-target effects, reducing potential side effects while improving therapeutic outcomes. Precision targeting guarantees peptides reach their intended destination, maximizing therapeutic impact. Advanced nanocarriers like liposomes and nanoparticles play a vital role by encapsulating peptides and guiding them to target sites.
Multiple strategies exist for achieving targeted delivery, including antibody, aptamer, and other targeting ligand applications. These ligands bind to specific cellular receptors, facilitating precise peptide delivery. Developing these targeting mechanisms constitutes a crucial aspect of peptide delivery system design, optimizing therapeutic results across various disease states.
Enhanced Stability
Peptides often face rapid degradation in bodily environments due to enzymatic activity. Delivery systems must address this instability to ensure bioactive peptides reach their targets. Protecting peptides from premature degradation presents a major challenge that innovative delivery systems help overcome. Approaches include chemical modifications to stabilize peptide structures, protective nanocarrier encapsulation, and stabilizer formulations.
Nanocarrier encapsulation provides protective barriers shielding peptides from degradation. These systems can also regulate peptide release, ensuring sustained, controlled delivery to target sites for more consistent therapeutic responses.
Controlled Release
Controlled release represents a vital component of peptide delivery systems, enabling sustained peptide release over extended periods. This sustained delivery can enhance therapeutic efficacy, reduce administration frequency, and minimize side effects. Precise release rate control ensures optimal therapeutic effects while minimizing adverse reactions. Various release mechanisms, including degradation-triggered or pH-triggered release, achieve desired release profiles.
Fine-tuning release rates proves essential for effective disease treatment. Controlled release also improves patient compliance by reducing required administrations, creating more manageable treatment regimens. Multiple factors influence release rates, including delivery system materials, peptide characteristics, and release mechanisms.
Improved Bioavailability
Enhancing peptide bioavailability stands as a primary objective in delivery system development. Bioavailability refers to the active peptide fraction reaching target sites. High bioavailability proves crucial for achieving desired therapeutic effects, with delivery systems playing a key role. These systems increase active peptide concentrations at target locations, enhancing efficacy while reducing required doses.
Various strategies aim to improve bioavailability, including specialized delivery vehicles and peptide sequence modifications. These approaches can reduce administration frequency and improve patient compliance, leading to more efficient therapeutic interventions. Formulation strategies enhancing bodily peptide stability also significantly contribute to improved bioavailability.
Time management is the practice of planning and exercising conscious control over the amount of time spent on specific activities. It is a skill that enhances productivity and efficiency, allowing individuals to maximize their output with the time available.
Challenges and Future Directions in Peptide Therapy Research
Optimizing Peptide Delivery
One of the significant hurdles in peptide therapy research involves achieving efficient, targeted peptide delivery to specific bodily sites. Unlike small molecule drugs, peptide therapeutics often face enzymatic degradation and rapid bloodstream clearance. Developing innovative delivery systems - including nanoparticles, liposomes, or biocompatible polymers - becomes essential for protecting peptides and enhancing bioavailability. This requires careful consideration of peptide modifications, conjugation strategies, and appropriate delivery vehicle selection to maximize therapeutic effects.
Addressing Immunogenicity
Peptide therapies risk triggering immune responses that may cause adverse effects and limit clinical applications. Understanding peptide immunogenicity and developing mitigation strategies proves essential. This involves characterizing immunogenic epitopes within peptide sequences and exploring methods to mask or modify these regions. Additional research into immune tolerance induction and peptide formulations minimizing immune activation remains crucial for successful peptide therapy translation.
Overcoming Peptide Stability
Peptide therapeutics frequently suffer from degradation, denaturation, and aggregation under physiological conditions, potentially reducing efficacy and shelf life. Strategies to enhance stability - including peptide backbone modifications, protective group incorporation, or stabilizing excipient use - prove vital for developing robust therapies. Careful consideration of peptide sequence, formulation, and storage conditions remains critical for preserving peptide integrity and activity.
Developing Novel Peptide Sequences
Identifying and designing novel peptide sequences with enhanced therapeutic properties continues as a major research focus. Computational tools and high-throughput screening technologies enable rapid exploration of peptide sequence space to identify promising candidates. This process typically involves studying existing peptide structural and functional characteristics to guide novel sequence design with improved target specificity, potency, and pharmacokinetic profiles. Novel sequences might target specific cellular pathways or serve as innovative therapeutic agents.
Enhancing Peptide Specificity and Target Engagement
Achieving high specificity and target engagement with peptide therapeutics proves critical for maximizing benefits while minimizing off-target effects. Specificity improvement strategies include developing peptide conjugates, incorporating targeting moieties, or utilizing peptide aptamers to enhance binding affinity and selectivity. This requires deep understanding of target protein structure and function, along with peptide sequence optimization to ensure specific interactions while minimizing unrelated protein or cellular interactions. Such advancements remain essential for minimizing side effects and maximizing peptide therapy efficacy.