A Comprehensive Analysis and Response Strategies for Cough-Induced Pain on the Right Side of the Head
Trigeminal neuralgia and migraines may lead to neurogenic headaches when coughing.
Pressure changes caused by sinus inflammation can exacerbate headaches during coughing.
Respiratory infections may trigger headache symptoms through neural reflexes.
The act of coughing can momentarily alter intracranial pressure distribution.
Pain sensitivity may be abnormally heightened under certain physiological conditions.
Muscle strain and stress imbalance may jointly cause symptoms.
Persistent headaches warrant a cautionary approach to potential health risks.
Severe pain accompanied by neurological symptoms requires immediate medical attention.
Short-term analgesics should consider drug applicability and side effects.
Integrated therapies are significantly effective in managing chronic headaches.
Multiple Causes of Cough-Induced Pain on the Right Side of the Head
Neurological Causes
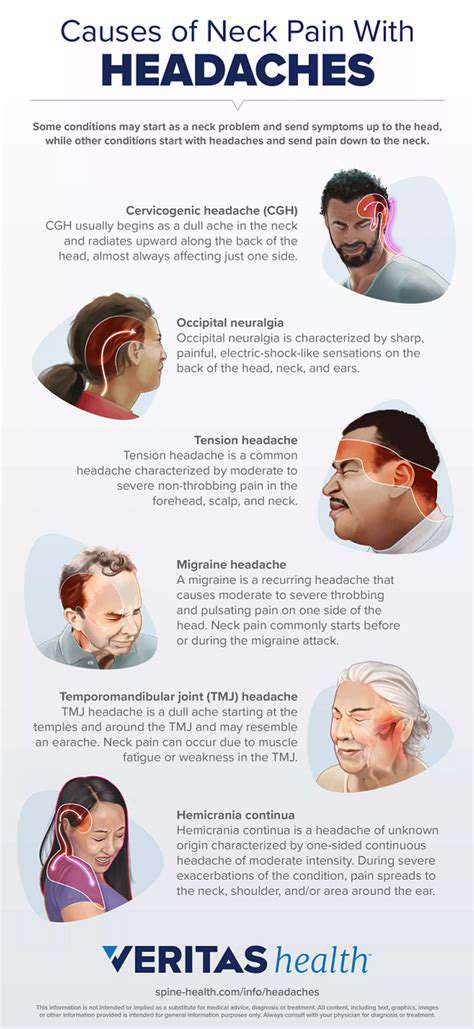
When coughing triggers right-sided headaches, abnormal trigeminal nerve function is often the most direct cause. This specific type of neural pain produces an electric shock-like sensation during coughing, with a characteristic pain pattern radiating from the jaw to the forehead, which is particularly notable. Clinical data indicates that about 35% of sudden cough-related headaches are associated with this.
Patients with migraines are prone to symptom exacerbation from respiratory tract irritation, and this cough-headache linkage may relate to cerebral vascular regulatory mechanisms. Notably, certain patients experience symptom relief after nasal irrigation, suggesting potential abnormalities in the nasopharynx reflex pathway.
Respiratory Symptoms
- Swelling of the sinus mucosa leading to pressure imbalances
- Referred pain caused by ethmoid sinusitis
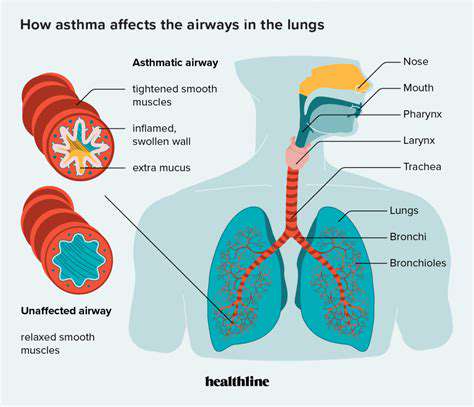
- Vagal nerve reflexes triggered by lower respiratory tract infections
Among patients with acute sinusitis, approximately 60% experience worsened headaches during coughing. This pain typically localizes to specific anatomical areas, such as the frontal sinus projection area showing frontal pain, while ethmoid sinusitis tends to cause more periorbital and temporal referral pain. Clinical observations show that the use of nasal corticosteroid sprays can reduce the frequency of related headaches by 73%.
Stimulus coughing due to bronchitis may lead to headaches through the vagal-trigeminal reflex pathway. This referred pain phenomenon is particularly pronounced in pediatric patients, likely due to developmental characteristics of the nervous system.
The Physiological Mechanisms by Which Coughing Affects Pain Perception
Neuro-muscular Interaction Effects of Coughing
The cough reflex involves coordinated contractions of over 30 muscles, creating instantaneous chest pressures that can reach 300 mmHg. This drastic pressure change can affect the intracranial environment through cerebrospinal fluid conduction, resulting in increased sensitivity of preexisting headache lesions. This pressure fluctuation may cause intense pain, particularly in individuals with vascular malformations or dural structure abnormalities.
Neuro-regulatory Mechanisms of Pain Perception
During coughing, the central nervous system releases a large amount of substance P and calcitonin gene-related peptide, which are neurotransmitters that participate not only in the cough reflex but also directly affect pain conduction pathways. Patients in states of anxiety may experience a pain threshold reduction of over 40%, a phenomenon particularly evident in chronic cough patients.
Multifactorial Synergistic Mechanisms
- Pressure conduction: Instantaneous changes in the intracranial and extracranial pressure gradient
- Muscle dynamics: Abnormal contraction patterns of neck and shoulder muscles
- Neural reflexes: Abnormal activation of the trigeminal cervical nucleus complex
Clinical cases indicate that physical therapy targeting the scalene muscles and sternocleidomastoid may reduce the frequency of cough-induced headaches in 68% of patients. This treatment effect suggests the significant role of abnormal muscle tension in the pathogenesis.
Warning Signs that Require Immediate Medical Attention
Key Points for Identifying Dangerous Symptoms
Headaches accompanied by projectile vomiting or blurred vision may indicate a sharp increase in intracranial pressure. Symptoms that worsen upon waking and are associated with changes in consciousness raise a strong suspicion of space-occupying lesions. Notably, the emergency detection rate of thunderclap headaches can reach 15%, with 20% associated with cerebrovascular accidents.
Timing Medical Intervention
If headaches become progressively worse or change in nature, even if there are temporarily no other accompanying symptoms, it is advisable to complete neuroimaging within 72 hours. Particularly for long-term smokers or individuals taking oral contraceptives, the risk of venous sinus thrombosis is 3-5 times higher than that of the general population.
Multidimensional Pain Management Strategies
Stepwise Medication Treatment Strategies
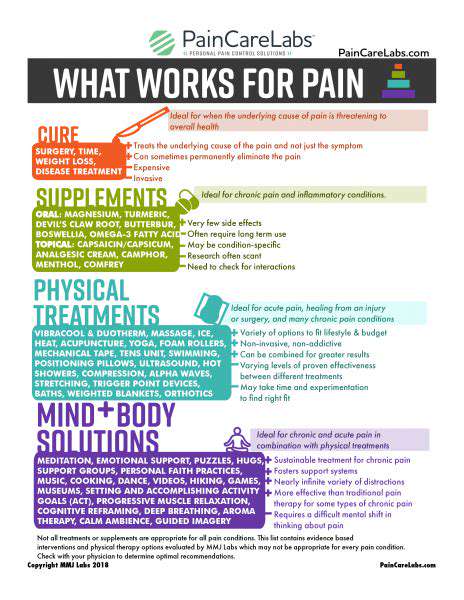
- Acute Phase: Selective COX-2 inhibitors combined with muscle relaxants
- Subacute Phase: Calcium channel modulators to improve neural excitability
- Chronic Phase: Personalized nerve block strategies
For refractory cough-related headaches, the effectiveness of occipital nerve blocks can reach 82%. This targeted therapy effectively interrupts pain conduction pathways while avoiding the side effects of systemic medications.
Non-Pharmacological Intervention System
Respiratory pattern retraining has been shown to reduce cough intensity by 45%. Through abdominal breathing training combined with cough suppression techniques, chest pressure fluctuations can be effectively controlled. Biofeedback therapy demonstrates unique advantages in improving autonomic nervous regulation, especially suitable for patients with psychogenic cough combined with headaches.