Comprehensive Analysis and Coping Strategies for Head and Neck Pain
Table of Contents
- Muscle tension caused by poor posture is a common trigger of head and neck pain
- Traumas such as whiplash can significantly worsen head and neck discomfort
- Chronic diseases like arthritis may develop into persistent pain
- Psychological stress may amplify the perception of pain
- Learning to recognize warning signs can help seize the golden time for medical treatment
- The synergistic analgesic effects of physical therapy combined with exercise
- Risk control of medication use and personalized medication plans
- Emergency handling principles for sudden severe pain
- Key points in managing chronic pain lasting more than three months
- Establishing a pain diary to track changes in condition
- Special handling procedures for symptoms accompanied by fever
- The application of multidisciplinary consultation in complex cases
- The golden balance between home care and professional treatment
- Six key dimensions for assessing treatment effectiveness
Analysis of Common Triggers for Head and Neck Pain
Muscle Tension Imbalance
Among modern office workers, over 68% of headache cases are related to compensatory contractions of neck muscles. When we maintain a forward-leaning posture while operating electronic devices for long periods, the trapezius and sternocleidomastoid muscles remain in a constant state of tension, leading to lactic acid buildup and localized circulation disorders. It is recommended to perform neck stretching exercises every 45 minutes, including chin retraction training and scapular squeezing exercises.
Management of Post-Traumatic Sequelae
- Whiplash due to motor vehicle accidents
- Cervical spine collisions in ball sports
- Strains caused by protective postures during falls
- Direct impact injuries to the head and neck
For example, in a traffic accident, the acceleration produced at the moment of collision can be equivalent to the head experiencing 7 times the force of gravity. This sudden external force can lead to tears in the cervical facet joint capsule and a sharp increase in intradiscal pressure. It is advised to undergo professional rehabilitation assessment within 72 hours after the injury to prevent annular tears from evolving into chronic pain.
Screening for Pathological Factors
Clinical statistics show that among patients over 50 with persistent neck pain, about 34% have undetected degenerative changes in the cervical spine. Warning symptoms such as morning stiffness lasting more than 30 minutes and night pain waking you up should be noted, as they may indicate systemic diseases like ankylosing spondylitis or rheumatoid arthritis.
Mind-Body Interactions
Patients with anxiety disorders generally show 42% higher surface electromyography values in neck muscles compared to healthy individuals, creating a vicious cycle of neuromuscular overactivation. Progressive muscle relaxation training combined with biofeedback therapy can reduce pain scores by 57%, and it is recommended to establish a pain-emotion diary within the framework of cognitive behavioral therapy to record symptom fluctuations in specific situations.
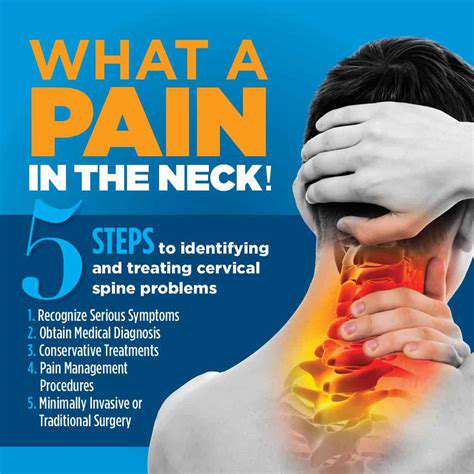
Symptom Identification and Grading Assessment
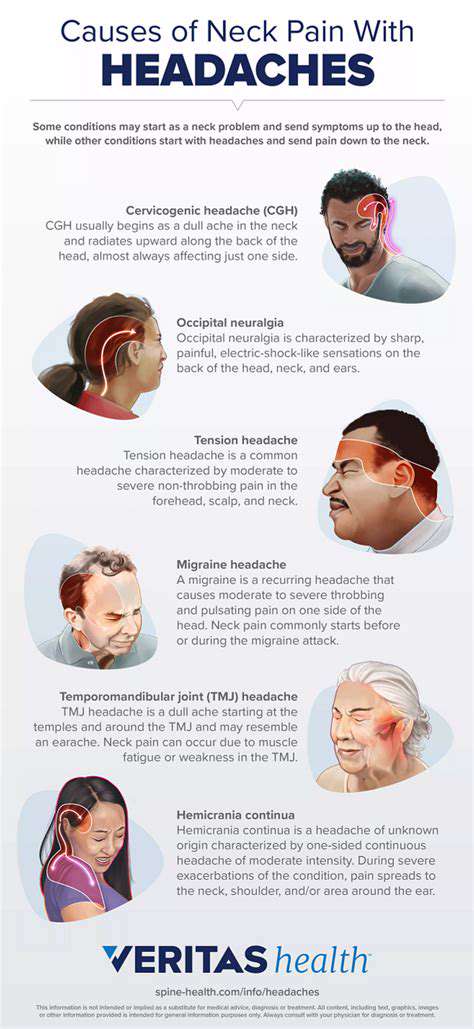
Characteristic Clinical Manifestations
Occipital neuralgia typically presents as electric shock-like pain at the back of the head, while cervicogenic headaches often manifest as unilateral pulsating pain in the temple area. It is important to note that neck pain accompanied by upper limb numbness suggests possible nerve root compression, which necessitates prioritizing cervical spine MRI examinations.
Identification of Warning Signs
Immediate medical attention is warranted when pain is accompanied by any of the following conditions:
- Sudden severe headache (thunderclap headache)
- Blurred vision or double vision lasting more than 2 hours
- Difficulties swallowing accompanied by hoarseness
- Progressively worsening balance disturbances
Application of Home Assessment Tools
The modified NDI (Neck Disability Index) scale is recommended for self-assessment, scoring on 10 dimensions including pain intensity, personal care, and lifting weights. A total score exceeding 15 suggests seeking professional rehabilitation treatment, while also recording factors related to pain onset and alleviation (such as specific postures, temperature changes, etc.).
Establishing a Stepwise Treatment System
Recent Advances in Physical Therapy
Suspension training therapy (SET) enhances the activation efficiency of deep neck flexors through open kinetic chain training. Combined with extracorporeal shock wave therapy, it effectively releases calcified fascia adhesion points. Recent studies show that this combined therapy can reduce VAS scores in chronic neck pain patients by 62%.
Precision in Medication Use
For neuropathic pain, the combination of gabapentin and selective COX-2 inhibitors is more effective than monotherapy. However, it is important to note that long-term use of NSAIDs may damage the gastrointestinal mucosa, so preventive protection with proton pump inhibitors is recommended.
Judging the Timing for Medical Intervention
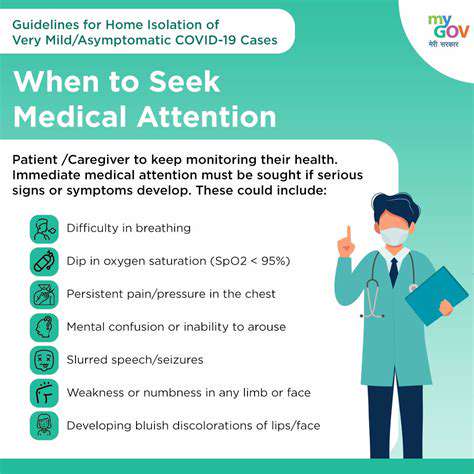
Emergency Indication Grasp
The emergency response protocol should be initiated in the following situations:
- Consciousness disturbances after trauma
- Cervical movement accompanied by symptoms of spinal shock
- Progressively worsening neurological deficits
Management of Chronic Conditions
A 3×3 follow-up pattern is recommended: efficacy evaluations should be conducted on the 3rd day, 3 weeks, and 3 months after the initial treatment. Effective treatment is indicated by:
- Reduction in pain frequency by >50%
- Improvement in daily activity limitation by >30%
- Decrease in analgesic dosage by >40%