Comprehensive Analysis of Frontal Pain: Causes and Coping Strategies
Article Outline
- Sinusitis often triggers frontal pain accompanied by nasal congestion and pressure sensation
- Cervicogenic headache originates from cervical spine issues leading to frontal discomfort
- Migraines commonly manifest as severe headache types concentrated in the frontal region
- Poor posture and stress-induced tension-type headaches affect the frontal area
- Medication overuse may trigger a rebound headache vicious cycle
- Emotional stress can significantly exacerbate frontal pain symptoms
- Specific warning symptoms require immediate medical examination
- Understanding the timing of various analgesics and alternative therapies
- Establishing daily prevention strategies to effectively manage recurrence issues
Common Triggers of Left Frontal Pain
Frontal Discomfort Caused by Sinusitis
When the sinus mucosa becomes inflamed, a noticeable pain sensation often occurs in the frontal region. This discomfort usually accompanies symptoms such as nasal blockage and facial pressure, and in severe cases, may even affect olfactory function. Clinical statistics indicate that about 15% of adults experience at least one acute sinusitis episode each year, especially common during seasonal changes.
Many patients describe the pain as significantly worsening when bending over or with changes in air pressure, sometimes easily mistaken for ordinary headaches. It is recommended to relieve symptoms through warm compresses or nasal irrigation; if symptoms persist for more than a week, medical consultation should be considered.
Traction Pain Due to Cervical Spine Issues
Cervicogenic headache primarily originates from abnormal cervical spine structure, with pain radiating along nerve pathways to the frontal area. This type of headache is often overlooked, and studies show that over 60% of chronic headache patients actually have cervical spine lesions. Improving neck muscle balance through physical therapy can effectively alleviate this type of traction pain.
It is advisable to avoid prolonged neck bending while using electronic devices and to perform neck stretching exercises every hour. If symptoms include numbness in the hands or blurred vision, immediate cervical spine imaging examination is recommended.
Characteristic Expression of Migraines
Typical migraines often present as unilateral pulsating severe pain, commonly concentrated around the eye sockets and the frontal area. Recent studies have found that about 38% of migraine patients experience pain primarily on the left side, possibly related to abnormal vasoconstriction. Keeping a record of diet and sleep conditions during episodes can help identify individual triggers.
It is noteworthy that some patients may experience prodromal symptoms such as visual flashes or olfactory sensitivity; these warning signals can serve as timing points for taking preventive measures. It is advisable to take prescription medications at the onset of symptoms, which can effectively shorten the duration of the attack.
Everyday Triggers of Tension-Type Headaches
Modern individuals often suffer from tension-type headaches caused by sustained muscle contractions in the head and neck due to fixed postures, making it a common occupational disease among office workers. In addition to adjusting desk and chair heights, it is recommended to perform shoulder and neck relaxation exercises every 30 minutes, along with deep breathing practices to relieve muscle tightness.
Clinical observations have found that these headaches often worsen in the afternoon, positively correlated with work fatigue levels. Using ergonomically supportive pillows can reduce the frequency of daily headaches by more than 40%.
The Adverse Effects of Medication Overuse
Frequent use of painkillers may lead to central nervous system sensitization, forming a vicious cycle of medication overuse headaches (MOH). It is important to note that continuous use of acetaminophen for more than 10 days/month or NSAIDs for more than 15 days/month can trigger such headaches.
The stepwise tapering method is recommended, along with non-pharmacological therapies for transition. Case studies have shown that combining cognitive behavioral therapy can reduce the recurrence rate to one-third of the original.
Symptom Interpretation and Risk Assessment
Warning Significance of Accompanying Symptoms
If frontal pain is accompanied by sudden vision loss, speech difficulties, or limb weakness, it may be a sign of a cerebrovascular accident. According to the American Heart Association guidelines, the golden period for intravenous thrombolysis treatment is within 4.5 hours of the onset of such symptoms; delay in seeking medical attention may lead to permanent neurological damage.
Also, nighttime awakening due to pain, unexplained weight loss, and other systemic symptoms should be noted, as these may indicate intracranial lesions or immune system diseases. Comprehensive health checks are recommended as soon as possible.
Key Points for Differentiating Pain Patterns
Different pain patterns suggest different underlying causes:
- Pulsating pain is more common in vascular headaches
- Continuous dull pain may indicate tension-type headaches
- Posture-related pain often hints at cervical spine issues
It is recommended to use a pain diary to record the time of onset, intensity (1-10 points), and alleviating factors, as providing this information to the physician during consultation can enhance diagnostic accuracy by over 70%.
Timing of Imaging Examinations
When the following conditions occur, physicians usually recommend brain MRI or CT scans:
- New onset headache over age 50
- Sudden change in pain characteristics
- Accompanied by cognitive decline
Recent imaging technologies can detect millimeter-level vascular changes, and early detection can effectively prevent 85% of hemorrhagic strokes from occurring.
Judging the Timing for Medical Attention
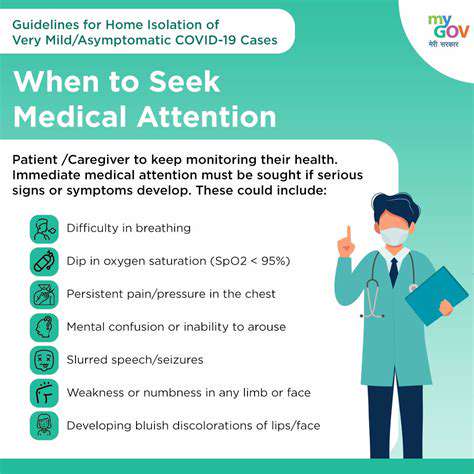
Danger Signs Needing Immediate Medical Attention
Thunderclap headache (sudden severe pain reaching maximum intensity) may be a manifestation of subarachnoid hemorrhage, with a mortality rate of 40%. Other danger signals include:
- Fever with neck stiffness
- Recent history of head trauma
- Progressively worsening morning headaches
Emergency physicians remind that if any of the above symptoms occur, one should promptly go to the emergency room, as delays in seeking medical attention may lead to irreversible consequences.
Situations for Suggested Outpatient Evaluation
If headaches show the following changes, it is advisable to arrange for a neurology outpatient visit within two weeks:
- Monthly frequency increases by more than 50%
- Poor response to standard pain relief medications
- Accompanied by newly appeared tinnitus symptoms
The physician may arrange for an EEG or vascular ultrasound to rule out rare causes such as temporal arteritis or cerebral venous thrombosis.
Diverse Treatment Options Analysis
Rational Application of Pharmacological Treatment
During the acute phase, one may choose nonsteroidal anti-inflammatory drugs (NSAIDs), but attention should be paid to:
- Patients with gastric ulcers should use it with gastric medication
- Patients with hypertension should avoid caffeine-containing combination preparations
Regarding preventive medications, the new CGRP antagonists can reduce the frequency of migraine attacks by up to 50%, but these need to be self-paid. It is recommended to discuss personalized medication strategies with a physician.
Scientific Evidence for Non-Pharmacological Interventions
Clinical studies have confirmed the significant effectiveness of the following methods:
- Transcranial magnetic stimulation (TMS) improves stubborn migraines
- Biofeedback training enhances autonomic nervous control
- Practicing Tai Chi reduces the frequency of tension-type headaches
Integrative treatment models combining multiple therapies can enhance overall effectiveness by over 30%, especially suitable for chronic recurrent patients.
Key Strategies for Daily Management
Establishing regular routines and stress management is fundamental:
- Maintain a fixed sleep cycle (deviation <30 minutes)
- Engage in progressive muscle relaxation training
- Supplement with magnesium ions and vitamin B2
Follow-up studies show that patients executing a complete prevention plan reduced their medication use by an average of 65% after one year, significantly enhancing their quality of life.