Các triệu chứng tự chủ đi kèm với đau đầu
Các triệu chứng tự chủ trong đau đầu căng thẳng
Đau đầu căng thẳng, một loại đau đầu phổ biến, thường đi kèm với một loạt các triệu chứng tự chủ. Những triệu chứng này, xuất phát từ th
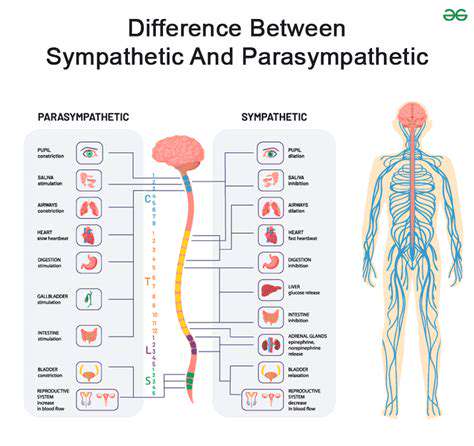
Những cân nhắc chẩn đoán về rối loạn tự chủ trong đau đầu
Đánh giá thần kinh
Một đánh giá thần kinh toàn diện là rất cần thiết để đánh giá rối loạn tự chủ trong đau đầu. Đánh giá này nên bao gồm một cuộc phỏng vấn chi tiết
Disclaimer: All articles on this site are original, please do not reprint