Table of contents
Poor posture causes head pain when leaning forward.
Stress and anxiety lead to tension headaches during physical stress.
Inflamed sinuses increase head pain when bending down.
Cervical spine disorders can cause discomfort when leaning forward.
Dehydration and nutrient deficiencies may trigger headaches.
Tension headaches often arise from muscle contractions in the upper body.
Eye strain contributes to head pain, especially from prolonged screen use.
Effective management includes physical therapy, hydration, and stress reduction strategies.
Common Causes of Head Pain When Leaning Forward
Posture-Related Tension
Poor posture is a leading cause of head pain, especially when leaning forward. As individuals position their bodies incorrectly, it puts undue strain on neck and shoulder muscles. This tension can lead to muscle fatigue, thereby triggering headaches that often intensify with certain movements.
When leaning forward, many people tend to hunch their shoulders or crane their necks. This unnatural alignment can contribute to cervical spine issues. Over time, this strain results in discomfort that mimics headache symptoms, making it essential to maintain proper posture.
Stress and Anxiety
Stress and anxiety are common culprits behind tension headaches that manifest when leaning forward. In moments of increased mental pressure, the body tends to tighten muscles, particularly in the neck and scalp. This response can exacerbate head pain, particularly in scenarios where one is physically leaning.
Sinus Issues
Sinus infections or chronic sinusitis can lead to significant discomfort in the head, particularly when leaning forward. When the sinuses become inflamed, pressure builds within the sinus cavities, leading to pain that can radiate to the forehead and temples. This sensation often worsens when tilting the head downward.
Cervical Spine Disorders
Issues related to the cervical spine, such as herniated discs or arthritis, can manifest as head pain when leaning forward. The cervical vertebrae are connected to head and neck functions, meaning any misalignment can lead to pain radiating to the head. When the head is tilted forward, it can increase pressure on these areas, leading to exacerbated discomfort.
Dehydration and Nutritional Deficiencies
Dehydration is often overlooked as a cause of head pain, especially when leaning forward. Insufficient water intake can lead to diminished blood flow to the brain, resulting in headaches. The position of leaning forward might compound these outcomes, causing increased discomfort during physical tasks or activities.
1. Sinusitis
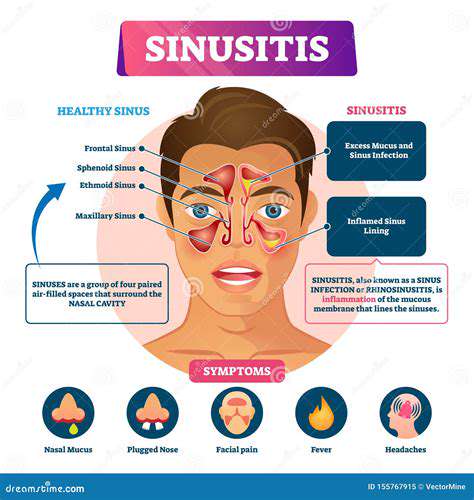
1.1 Understanding Sinusitis and Its Symptoms
Sinusitis, commonly referred to as a sinus infection, occurs when the nasal cavities become swollen or inflamed. This condition can stem from infections, allergies, or autoimmune issues. The primary symptoms of sinusitis include facial pain, nasal congestion, and a reduced sense of smell. In many cases, individuals may also experience pressure around the eyes, cheeks, and forehead.
People suffering from sinusitis often describe the discomfort as a persistent headache that intensifies with certain movements, particularly when leaning forward. Additionally, sinusitis can lead to a buildup of mucus, which may contribute to feelings of fullness in the head. This can result in increased pain and pressure, significantly impacting one's quality of life.
Recognizing the symptoms of sinusitis is crucial for timely treatment. Many individuals may overlook initial signs or assume they are just suffering from a common cold. Left untreated, sinusitis can progress from acute to chronic, leading to long-term issues and frequent bouts of pain. Therefore, awareness and early intervention are important in managing this condition.
1.2 Causes and Risk Factors for Sinusitis
Sinusitis can arise from a variety of causes, including viral infections, bacterial infections, allergies, and pollution. Blockage of the sinus cavities is often the primary reason for inflammation and infection. Understanding the triggers that lead to sinusitis can help individuals avoid situations that may compromise their sinus health. Common allergens such as dust, pollen, and pet dander can significantly contribute to the onset of sinus issues.
Another risk factor includes structural abnormalities within the nasal passages, such as a deviated septum or nasal polyps. These structural issues can impede normal drainage of the sinuses, creating an environment ripe for infection. Additionally, environmental factors, such as exposure to smoke, strong odors, or pollutants, can exacerbate sinus problems.
Individuals with a history of asthma or allergic rhinitis are also more likely to develop sinusitis. Understanding your personal health background, along with potential environmental triggers, can be key in preventing recurrent sinus issues. By identifying these factors, individuals can take proactive measures to minimize the risk of sinus infections.
1.3 Diagnosis and Treatment Options for Sinusitis
Diagnosing sinusitis typically involves a combination of a physical examination and imaging tests. A healthcare provider may check for physical signs, such as nasal inflammation or discharge. In some cases, a CT scan may be ordered to evaluate the sinuses for structural abnormalities. These diagnostic approaches ensure that the appropriate treatment plan can be developed based on the underlying cause of the sinusitis.
Treatment options vary depending on the severity and cause of the sinusitis. For acute cases, over-the-counter medications like decongestants or pain relievers may offer relief. In more severe cases, antibiotics may be prescribed, particularly if a bacterial infection is suspected. Additionally, antihistamines can help alleviate symptoms related to allergies, contributing to a decrease in inflammation.
For chronic sinusitis, a more comprehensive approach may be required, which could include trials of nasal corticosteroids or surgery for anatomical correction. Surgical options should be considered a last resort but can provide significant relief for those with persistent issues. A collaborative approach between patient and healthcare provider is essential in determining the most effective treatment strategy.
1.4 Preventive Measures to Avoid Sinusitis
Preventing sinusitis often involves managing risk factors and maintaining overall health. Individuals can reduce their risk by staying hydrated, keeping nasal passages moist, and using humidifiers in dry environments. Practicing good hygiene, such as regular handwashing and avoiding close contact with infected individuals, can also play a significant role in prevention. These simple steps can help reduce the chances of contracting respiratory infections that may lead to sinusitis.
Allergy management is another key preventive strategy. For those susceptible to allergens, identifying and avoiding triggers is critical. Using air purifiers, keeping windows closed during high pollen seasons, and regular cleaning to minimize dust and pet dander can significantly decrease exposure. Such proactive measures can lessen the likelihood of sinusitis flare-ups linked to allergic reactions.
Lastly, routine check-ups with a healthcare provider can help monitor and manage any underlying health issues that may contribute to sinusitis. By addressing health issues like asthma or allergies early on, individuals can minimize the risk of complications such as recurrent sinus infections. Taking charge of personal health can lead to effective management and promotion of well-being regarding sinus conditions.
2. Tension Headaches
Understanding Tension Headaches
Tension headaches are one of the most common types of headaches, often described as a sensation of pressure or tightness around the head. This discomfort can range from mild to moderate and is frequently accompanied by neck and shoulder tension. These headaches typically arise from a combination of muscle contractions in the head, neck, and shoulders, which can be triggered by various lifestyle factors, stress, or poor posture.
It’s important to recognize tension headaches early to prevent them from escalating. While some individuals may only experience them occasionally, others might find that they happen frequently, particularly in challenging or stressful situations. Understanding the underlying causes and identifying potential triggers is crucial for effective management of this type of headache.
Common Symptoms of Tension Headaches
The symptoms associated with tension headaches can vary significantly among individuals. Commonly, sufferers may report a dull ache on both sides of the head, which may feel like a tight band constricting the skull. Unlike migraines, tension headaches generally do not involve nausea, vomiting, or sensitivity to light and sound, making them somewhat easier to manage in daily life.
Additionally, individuals dealing with frequent tension headaches may also experience increased muscle tightness in the neck and shoulders. This leads to systemic discomfort that can further exacerbate the headache. Recognizing these symptoms can aid individuals in seeking appropriate medical advice and adopting preventive measures.
Management and Treatment Options
Effective management of tension headaches often involves both lifestyle changes and medical interventions. Simple strategies such as using proper ergonomics while working, improving posture, and engaging in regular physical activity can significantly reduce the frequency and intensity of these headaches. Incorporating relaxation techniques such as deep-breathing exercises, yoga, or meditation is also beneficial.
When lifestyle changes are insufficient, over-the-counter pain relief medications, such as ibuprofen or acetaminophen, can be effective. However, it’s essential to consult with a healthcare professional before beginning any medication, especially for those who experience chronic headaches, to avoid dependency and assess for other underlying conditions.
When to Seek Medical Attention
Although tension headaches are typically manageable with self-care and over-the-counter treatments, it’s important to be vigilant about when to seek medical attention. If headaches become more severe, change in pattern, or are accompanied by neurological symptoms such as visual disturbances or significant changes in coordination, these could indicate a more serious condition that requires immediate evaluation.
Additionally, if tension headaches are occurring more than 15 days a month, it may be time to consult with a healthcare provider. They can provide a comprehensive assessment, determine if there are other contributing factors, and help develop a tailored treatment plan that may involve physical therapy, counseling, or alternative therapies for optimal headache management.
3. Cervicogenic Headaches
Understanding Cervicogenic Headaches
Cervicogenic headaches are a common type of headache that originates from the cervical spine, which comprises the neck region. These headaches typically occur due to issues within the neck, such as muscle tension, disc herniation, or spinal abnormalities. Unlike migraines or tension headaches, cervicogenic headaches can often be traced back to a single traumatic event or chronic neck dysfunction. Understanding the underlying causes is essential for effective treatment and management of this condition.
Individuals suffering from cervicogenic headaches may experience pain that radiates from the neck and often travels to the front of the head. The discomfort can sometimes resemble migraines but usually lacks the associated symptoms like nausea or visual disturbances. It can be exacerbated by certain positions, such as leaning forward, which places additional strain on the cervical spine. Identifying the specific triggers and symptoms can greatly enhance the effectiveness of treatment plans.
Diagnosis of cervicogenic headaches usually involves a thorough evaluation, including a review of medical history, physical examination, and potentially imaging studies to assess cervical spine structure. Healthcare professionals often look for referred pain patterns that are characteristic of cervicogenic headaches, and ruling out other headache types is crucial to ensure that the correct treatment measures are taken.
Common Causes and Risk Factors
Cervicogenic headaches can be linked to various risk factors, with poor posture being one of the most significant contributors. Many people spend long hours hunched over computers or mobile devices, which places undue stress on the neck muscles and joints. Over time, this can lead to structural changes in the cervical spine, prompting the development of headache symptoms that hinder daily activities and overall quality of life.
Injury and trauma, such as whiplash from car accidents or falls, can also instigate cervicogenic headaches. The sudden movement can strain the muscles and ligaments in the neck, leading to inflammation and discomfort that manifests as headaches. Additionally, degenerative conditions like arthritis can contribute to these headaches by causing joint inflammation and nerve irritation in the cervical region.
Another important factor to consider is the influence of emotional stress. Tension and anxiety can lead to muscle tightness in the neck, further compounding existing issues and contributing to headache severity. Effective management often requires addressing both physical and psychological components in tandem, making a comprehensive treatment plan vital for long-term relief.
Effective Treatment and Management Strategies
Management of cervicogenic headaches often entails a multi-faceted approach combining medication, physical therapy, and lifestyle modifications. Over-the-counter pain relievers, such as ibuprofen and acetaminophen, may provide immediate relief, but they do not address the root causes of neck dysfunction. Long-term solutions often require more than just temporary pain management through medication.
Physical therapy is an effective treatment option, as therapists can develop targeted exercises that improve neck strength and flexibility. Techniques such as manual therapy, postural training, and ergonomic advice for workplace settings can significantly alleviate symptoms. Regular sessions can help individuals restore normal neck function, reduce pain intensity, and prevent future episodes of cervicogenic headaches.
In addition to professional therapy, lifestyle changes play a crucial role in management. Incorporating regular exercise, practicing good posture, and engaging in stress-reduction techniques such as yoga or meditation can all contribute to a decrease in headache frequency and intensity. It's important for individuals to remain proactive about their health and seek guidance from healthcare providers when needed to tailor the best strategies for their specific condition.
4. Migraines
Understanding Migraines: Symptoms and Triggers
Migraines are not just simple headaches; they are complex neurological events that can significantly disrupt daily life. These intense headaches are often accompanied by a range of symptoms, including nausea, vomiting, and extreme sensitivity to light and sound. Understanding these symptoms is critical for effective management and seeking appropriate care.
Common triggers for migraines can include stress, hormonal changes, certain foods, and changes in sleep patterns. Identifying personal triggers is essential for individuals prone to migraines, as this awareness can lead to proactive measures in avoiding potential attacks. Keeping a migraine diary can be a useful strategy for tracking patterns and associations.
Additionally, genetics can play a significant role in migraine frequency and severity. Those with a family history of migraines are often more susceptible, which highlights the importance of understanding both environmental and hereditary factors when addressing this condition.
Lastly, it should be noted that not all headaches are migraines. It is crucial to differentiate between various types of headaches to ensure that individuals receive the correct diagnosis and treatment options. A healthcare provider can perform a thorough evaluation to determine the nature and cause of recurring head pain.
Migraine Management: Treatment Options and Lifestyle Adjustments
Effective management of migraines often involves a multi-faceted approach, including medications, lifestyle changes, and alternative therapies. While over-the-counter pain relievers may provide relief for mild headaches, prescription medications such as triptans or preventative therapies may be required for more severe migraines. Consulting with a healthcare provider to find the most effective medication regimen is crucial for long-term management.
Incorporating lifestyle adjustments can significantly reduce the frequency and intensity of migraines. Regular exercise, maintaining a consistent sleep schedule, and practicing stress-reduction techniques such as yoga or meditation can all lead to improved outcomes. Furthermore, dietary modifications, including the elimination of known triggers like aged cheeses or processed foods, can also be beneficial in a migraine management plan.
Alternative treatments such as acupuncture, biofeedback, and cognitive-behavioral therapy have shown promise in helping some individuals manage their migraines. These approaches often focus on holistic care, addressing both physical and emotional aspects of the condition to foster overall well-being and reduce migraine occurrences.
Finally, keeping open lines of communication with healthcare professionals facilitates a tailored treatment plan that meets individual needs. Regular check-ins with a doctor can help adapt treatment strategies as an individual's condition evolves, ensuring that the best possible care is maintained over time.
5. Eye Strain
Understanding Eye Strain and Its Connection to Head Pain
Eye strain, often referred to as asthenopia, can result from a variety of factors, including prolonged screen time, inadequate lighting, and poor posture. This discomfort often manifests as a dull or aching feeling around the eyes, which can be exacerbated when leaning forward or straining to focus. In our digital age, many people spend significant hours staring at computer screens, which increases the likelihood of developing eye strain symptoms.
When individuals lean forward, they may unknowingly alter their visual habits, putting additional stress on the eye muscles. This position often requires increased effort for the eyes to maintain focus, leading to a buildup of tension not only in the eyes but also radiating towards the head, further contributing to head pain. Thus, understanding the connection between posture and eye strain is crucial for identifying the underlying causes of discomfort.
Symptoms of eye strain can vary from person to person but commonly include dry eyes, blurry vision, headaches, and increased sensitivity to light. In many cases, these symptoms intensify when one is leaning forward while trying to read or use digital devices, making it essential to recognize the relationship between body posture and eye wellness. Addressing eye strain early can help minimize its impact on overall health and well-being.
Routine breaks, appropriate lighting, and ergonomic adjustments can significantly reduce the risk of developing eye strain. Eye strain prevention strategies, such as the 20-20-20 rule, which advises looking at something 20 feet away for 20 seconds every 20 minutes, can be particularly beneficial. By understanding the full scope of eye strain and its implications for head pain, individuals can take proactive steps to alleviate discomfort.
Effective Strategies to Alleviate Eye Strain and Head Pain
To effectively reduce eye strain and, consequently, head pain, adopting a holistic approach is key. One of the first steps is ensuring an ergonomic workspace that promotes better posture while minimizing strain on the eyes. This includes positioning the computer screen at eye level, using a chair that supports the back, and ensuring adequate distance from the screen. Small adjustments can have a tremendous impact on reducing the discomfort associated with leaning forward.
Another crucial strategy is optimizing lighting conditions. Working in a well-lit environment or using blue light filters on screens can significantly alleviate eye strain. Proper lighting reduces glare and prevents overstimulation of the eyes, making it easier to focus. Furthermore, incorporating regular eye examinations can help identify any vision issues that may be contributing to strain and addressing those proactively can prevent long-term problems.
Incorporating consistent breaks into the work routine is another practical solution. Stepping away from screens or engaging in relaxing eye exercises can relieve strain and ease tension headaches. Simple practices such as rolling your eyes, focusing on distant objects, or gently massaging around the eyes can effectively refresh the visual system and prevent discomfort.
Finally, staying well-hydrated and maintaining a balanced diet rich in nutrients that support eye health is vital. Foods rich in omega-3 fatty acids, vitamins C and E, and antioxidants can help maintain eye function and reduce the likelihood of strain. A combination of lifestyle changes, ergonomic adjustments, and regular self-care is essential for effectively managing both eye strain and associated head pain.
Strategies and Solutions for Relief
Identifying Common Causes of Head Pain When Leaning Forward
Understanding the underlying causes of head pain, particularly when leaning forward, is essential for effective relief. There are several potential triggers that can induce discomfort, including tension headaches, sinus issues, and even cervical spine problems. Each of these causes necessitates a tailored approach to treatment and management.
Tension headaches are often caused by muscular tension in the neck and scalp. When leaning forward, this tension can become exacerbated, leading to increased pain. Identifying the triggers for these headaches, such as stress or poor posture, can be crucial to mitigating future episodes.
Sinus issues can also manifest as head pain, particularly when bending the head at awkward angles. Allergies or infections can lead to sinus pressure, causing discomfort that intensifies when the head is positioned forward. Awareness of seasonal changes and maintaining good nasal hygiene can aid in managing these symptoms effectively.
Cervical spine problems should not be overlooked as a potential cause of head pain. Poor ergonomics during everyday activities, such as prolonged computer use, can significantly affect spinal alignment. Consultations with healthcare professionals may help identify if these structural issues are contributing to your discomfort when leaning forward.
Maintaining a head pain diary can be beneficial in tracking when and how often these headaches occur. Keeping detailed notes on posture, activity levels, and triggers will provide valuable information to healthcare professionals, enabling them to tailor an effective treatment plan based on individual needs.
Effective Strategies for Managing Head Pain
Implementing effective strategies to manage head pain requires a comprehensive approach, incorporating both preventative measures and reactive solutions. Regular exercise is a powerful tool that not only strengthens the neck muscles but also promotes overall well-being. Engaging in activities like yoga or pilates can enhance flexibility and relieve muscular tension.
Another crucial aspect of managing head pain is addressing posture—both your body position during daily activities and your workstation setup. Adjustments such as using ergonomic chairs, standing desks, or even supportive neck pillows can alleviate strain on your spine and reduce the frequency of headaches.
Hydration also plays a vital role in headache management. Dehydration is a common headache trigger, so ensuring that you're drinking sufficient water throughout the day is essential. Incorporating hydrating foods like fruits and vegetables can boost overall fluid intake and contribute to headache prevention.
Stress management techniques can significantly reduce the likelihood of tension headaches. Engaging in regular mindfulness practices, such as meditation or deep breathing exercises, can decrease stress levels and improve focus. Making these practices a part of your daily routine can yield long-term benefits.
Lastly, if head pain persists despite implementing these strategies, it's advisable to seek consultation from a healthcare professional. This can help to establish if additional interventions, such as medications or physical therapy, are necessary to provide ongoing relief.
Natural Remedies and Home Treatments for Head Pain
Exploring natural remedies and home treatments for head pain can provide considerable relief and empower individuals to manage their symptoms effectively. Among these remedies, herbal teas, particularly peppermint and ginger tea, have been reported to have soothing properties that may alleviate headache symptoms.
Another beneficial approach is the use of essential oils. Lavender oil, for instance, demonstrates calming effects and can be inhaled or applied to pressure points for relief. The aromatherapy benefits of certain essential oils can also aid in reducing stress and relaxing tense muscles, thus relieving headache pain.
Applying a cold or warm compress to the forehead or neck can significantly lessen headache discomfort. Cold packs can minimize inflammation and numb the pain, while warm compresses promote relaxation of tense muscles. Experimenting with both methods can help in identifying which offers greater relief for individual headaches.
Acupressure is an ancient practice that combines traditional Chinese medicine with pain relief. Pressing specific points on the body can release tension and alleviate pain. Learning about and practicing acupressure techniques at home can empower individuals to find relief quickly when symptoms develop.
Lastly, dietary adjustments may also contribute to reducing the frequency and intensity of headaches. Identifying potential food triggers, such as aged cheeses or processed meats, can provide insight into dietary modifications that promote better health and fewer headaches.
Professional Solutions and When to Seek Help
Understanding when to seek professional help is critical in managing head pain effectively. If headaches become recurrent or increasingly severe, it may signal an underlying health issue that requires the expertise of a healthcare professional. Early intervention can often lead to more effective treatment.
Healthcare providers can offer several solutions, from prescription medications to physical therapy, to specifically address the causes of head pain. Many healthcare professionals recommend a multidisciplinary approach, collaborating with specialists in neurology, physical therapy, and even nutrition to create a comprehensive treatment plan.
Moreover, diagnostic testing may be necessary if headaches are accompanied by additional symptoms, such as visual disturbances or neurological changes. Imaging studies can provide insight into potential structural issues influencing head pain, allowing healthcare providers to tailor treatment accordingly.
For chronic headache sufferers, cognitive behavioral therapy (CBT) can be beneficial. This psychological approach informs individuals about how thoughts and behaviors influence pain perception. Engaging in CBT may result in long-term changes in how one experiences pain, reducing the frequency and severity of headaches.
Ultimately, effective management of head pain often requires a combination of self-care strategies and professional intervention. By understanding the importance of timely medical support and exploring various treatment options, individuals can take charge of their health and enhance their quality of life.
1. Manage Sinus Issues
Understanding Sinus Anatomy and Function
The sinuses are air-filled spaces located within the facial bones, primarily designed to reduce the weight of the skull and enhance vocal resonance. These cavities are lined with a mucous membrane that produces mucus to trap pathogens and allergens, while also humidifying the air we breathe. Understanding the basic structure of the sinuses, including the maxillary, frontal, ethmoid, and sphenoid sinuses, is crucial for identifying the source of pain when leaning forward.
Sinus cavities play an essential role in respiratory health, but when they become inflamed due to infections or allergies, they can cause significant discomfort. Sinusitis is an inflammation of the sinus membranes, which can block drainage and create pressure. This pressure often exacerbates head pain when leaning forward, as the shift in position affects the fluid dynamics within the sinus cavities.
Moreover, the connection between the sinuses and the nasal passages means that any inflammatory response can lead to congestion and blockage, severely impairing airflow. Understanding how the anatomy of the sinuses affects overall sinus health can provide insight into some of the common causes of head pain associated with leaning forward.
Common Symptoms of Sinus Issues
Recognizing the symptoms associated with sinus problems is vital for effective management. Common symptoms include facial pain or pressure, particularly around the forehead and cheeks, which can intensify when bending forward. This pain occurs due to the increased pressure in the sinus cavities, making simple movements feel uncomfortable and alarming.
In addition to pain, individuals with sinus issues often experience nasal congestion, thick nasal discharge, and reduced sense of smell. These symptoms can significantly affect daily activities, contributing to feelings of fatigue or general malaise. If these symptoms last beyond a week or two, they may require medical attention to avoid worsening conditions.
Headaches are another prevalent symptom associated with sinus problems. They tend to feel like a dull ache that can become more pronounced with forward bending or during changes in position, indicating a relationship between sinus pressure and head pain. Recognizing these symptoms can aid in differentiating sinus-related pain from other types of headache, leading to more informed management strategies.
Effective Treatment and Management Strategies
Managing sinus-related issues often begins with a combination of self-care and medical treatment. Over-the-counter medications, such as decongestants and antihistamines, can be effective in reducing swelling and promoting drainage, alleviating pain when leaning forward. Nasal sprays and saline irrigation may also be recommended to soothe irritated tissues and improve mucous clearance.
For chronic sinusitis or persistent cases where standard treatments fail, healthcare providers may prescribe stronger medications, including nasal corticosteroids or antibiotics if a bacterial infection is suspected. Understanding treatment options gives patients the ability to make informed decisions about their health and engage in discussions with their healthcare provider regarding the most suitable therapies for their specific conditions.
Moreover, lifestyle modifications play a crucial role in managing sinus health. Staying hydrated, maintaining a clean environment free from allergens, and utilizing a humidifier can facilitate better sinus function and potentially reduce episodes of head pain. Avoiding triggers, such as smoke and strong odors, is also essential for maintaining optimal sinus health and improving quality of life.
2. Correct Posture
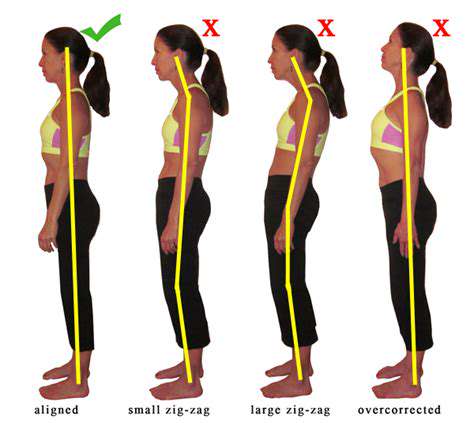
Understanding the Importance of Correct Posture
Correct posture plays a crucial role in maintaining overall health and wellness, particularly when it comes to preventing head pain. When we slouch or lean forward incorrectly, it can lead to excessive strain on the muscles of the neck and upper back. This strain may eventually result in tension headaches or exacerbated pain when leaning forward.
Moreover, the way we hold our bodies influences the alignment of the spine, which directly impacts nerve health. A well-aligned spine reduces the risk of nerve compression, allowing for optimal blood flow and function throughout the body. This is especially vital for anyone who spends hours at a desk or engaged in activities requiring prolonged periods of leaning.
It’s essential to be mindful of your posture not just while sitting, but also when standing or walking. Adopting a neutral spine position can alleviate unnecessary stress on the cervical structures. Regular practice of posture correction can literally reshape our bodies and improve how we move through our daily lives.
Incorporating posture checks throughout the day can be beneficial for overall comfort and health. Simple reminders or tools, like ergonomic furniture, can encourage us to maintain better alignment. Ultimately, correct posture is not just about aesthetics; it's about functional well-being and harmony within the body.
Common Posture Mistakes that Lead to Head Pain
Many individuals are unaware of the detrimental effects certain postural habits can have on their bodies. For example, leaning forward while working on a computer can cause the head to be positioned far beyond the shoulders. This forward head posture can increase the load on the neck muscles, leading to chronic head pain.
Another common mistake is sitting for extended periods without proper lumbar support. When the lower back is unsupported, it can create a domino effect, negatively influencing the rest of the spine and ultimately leading to discomfort in the head. To combat this, utilizing chairs that offer adequate support is essential for reducing stress on the musculoskeletal system.
Using mobile devices can also encourage poor posture habits. People often hunch over their phones for extended periods, which can strain neck muscles and contribute to tension headaches. Understanding these habits is the first step in identifying and correcting the postural issues that lead to head pain.
Lastly, infrequent breaks can exacerbate poor posture-related pain. Remember to stand up, stretch, and realign your body at regular intervals. Simple exercises to promote blood circulation and stretch tight muscles can mitigate the discomfort caused by poor posture.
Solutions and Strategies for Improving Posture
Improving posture begins with awareness of one’s own body mechanics during daily activities. Practicing mindful posture correction involves regularly checking in with your body to ensure it is aligned properly. Simple techniques, such as drawing your shoulders back and engaging your core, can profoundly impact your overall posture. Integrating these small adjustments into your routine can prevent discomfort as you lean forward.
Engaging in targeted exercises can also promote better posture. Strengthening the muscles that support the spine, including the core, back, and shoulders, can create a more balanced physique. Activities like yoga, pilates, and strength training are particularly effective in enhancing postural strength and stability.
Additionally, utilizing ergonomic tools such as standing desks, lumbar rolls, or neck-supporting cushions can significantly reduce your risk of developing head pain. These tools are designed to encourage a healthier body alignment and reduce strain. Investing in such equipment is a small price for the long-term benefit of improved comfort and health.
Lastly, consider working with a physical therapist or a qualified chiropractor. These professionals can provide personalized assessments and create a tailored plan to modify your posture effectively. Developing a consistent routine that incorporates all these strategies can lead to lasting relief from head pain associated with posture.
3. Physical Therapy
3.1 Understanding Physical Therapy in Treating Head Pain
Physical therapy plays a pivotal role for individuals experiencing head pain, particularly when leaning forward. The therapeutic modalities employed in a well-balanced physical therapy regimen can alleviate discomfort and improve mobility. By focusing on specific movements and exercises, patients can learn to manage their pain effectively and function more freely in their daily activities.
A comprehensive assessment is essential in physical therapy, enabling practitioners to identify the underlying causes of head pain. This thorough evaluation helps in developing a personalized treatment plan that addresses not only the symptoms but also the root of the problem, paving the way for long-term relief and improved quality of life.
3.2 Common Physical Therapy Techniques for Head Pain Relief
There are several techniques used in physical therapy that target head pain when leaning forward. One common approach is manual therapy, which involves hands-on manipulation of the body to relieve tension in the neck and shoulders. This technique can improve circulation and reduce muscle stiffness, helping to alleviate associated headaches and discomfort.
Another effective method is the use of therapeutic exercises. These exercises are tailored to strengthen the muscles supporting the head and neck, enhancing posture and reducing the likelihood of pain exacerbating during specific movements. Regular practice of these exercises can lead to significant improvements in both strength and mobility.
3.3 The Role of Posture in Head Pain Management
Posture is a critical factor in addressing head pain when leaning forward. Poor posture can strain the muscles and ligaments of the neck, leading to discomfort that manifests as headaches. Physical therapists often emphasize the importance of maintaining good posture to prevent unnecessary stress on these areas.
3.4 The Importance of Stretching and Strengthening Exercises
Stretching and strengthening exercises serve as fundamental components of physical therapy for head pain relief. Regular stretching helps to alleviate tension in the muscles of the neck and upper back, promoting relaxation and enhancing flexibility. This can lead to decreased instances of pain when leaning forward, as tight muscles are often responsible for triggering discomfort.
Strengthening exercises, on the other hand, help build the muscle support around the head and neck. A well-balanced musculature can stabilize the spine and reduce the risk of pain related to poor posture. By integrating both stretching and strengthening into a physical therapy program, patients can achieve a more holistic approach to managing their head pain effectively.
3.5 Seeking Professional Guidance in Physical Therapy
While self-treatment techniques may provide temporary relief, seeking professional guidance in physical therapy is essential for comprehensive care. A trained physical therapist can offer invaluable insights tailored to an individual's specific condition, ensuring that the exercises and techniques employed are safe and effective.
Additionally, professional physical therapy can facilitate the monitoring of progress and adjustments to the treatment plan as needed. This level of personalized attention allows patients to navigate their head pain journey with confidence, ultimately leading to a better understanding of how to manage their symptoms long-term.
4. Migraine Management
Understanding the Triggers of Migraines
Migraines can result from a multitude of triggers that vary significantly from person to person. Identifying these triggers is essential for developing a comprehensive management plan. Common triggers include stress, hormonal changes, certain foods, and environmental factors, which can all initiate a migraine episode. Keeping a detailed diary can be useful in recognizing patterns and specific triggers that exacerbate the migraines.
In some cases, physical factors such as neck strain or poor posture can lead to increased susceptibility to migraines. Leaning forward can create tension in the neck and shoulders, complicating existing conditions. Understanding how physical positioning interacts with migraine triggers can serve as a vital step toward optimized management.
Additionally, lifestyle choices play a crucial role in the frequency and intensity of migraines. Factors such as hydration, sleep quality, and regular meals contribute significantly. For instance, dehydration can amplify migraine symptoms, making it even more detrimental for those prone to head pain when leaning forward.
Moreover, external forces like bright lights, strong smells, or loud sounds can precipitate migraines in sensitive individuals. Evaluating and modifying your environment might provide relief and decrease the likelihood of experiencing migraines, transforming your living or working spaces into headache-free zones.
Effective Medicinal Treatments
When managing migraines, various medicinal treatments can be utilized based on the severity and frequency of episodes. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can provide quick relief for mild to moderate migraines. However, these should be taken with caution, as overuse can lead to rebound headaches.
For more severe migraines, prescription medications like triptans are often recommended as they specifically target migraine pain pathways. These medications can be beneficial for many patients seeking rapid relief from debilitating migraine symptoms. Consulting with a healthcare provider for appropriate dosage and frequency is essential to avoid potential side effects.
Additionally, preventative medications may be prescribed for individuals experiencing frequent or chronic migraines. Drugs such as beta-blockers or certain antidepressants can help reduce the frequency of attacks. Working closely with a doctor to establish a tailored preventative plan can significantly enhance quality of life for migraine sufferers.
Moreover, alternative medicinal options, including herbal supplements or acupuncture, are gaining popularity among individuals seeking holistic pain management methods. While these approaches require thorough research and professional consultation, they can complement traditional treatments effectively for some patients.
Lifestyle Adjustments for Improved Management
Implementing lifestyle adjustments can play a pivotal role in mitigating migraine occurrences and relieving symptoms. Regular exercise is one example that not only improves overall health but can also reduce stress levels that may trigger migraines. Engaging in activities like yoga or swimming can create a low-impact way to keep the body active without adding physical strain.
Dietary modifications are equally critical, as specific foods can either induce or alleviate migraines. Maintaining a balanced diet while being mindful of potential triggers, such as aged cheeses, processed meats, or artificial sweeteners, is essential. Keeping a food journal helps in identifying and eliminating these triggers effectively.
Furthermore, quality sleep is another vital factor. Establishing a consistent bedtime routine and ensuring 7 to 9 hours of sleep per night can improve restfulness. Inadequate or disrupted sleep patterns can exacerbate migraine disorders, making it crucial to prioritize sleep hygiene as part of a comprehensive management strategy.
Lastly, stress reduction techniques, such as mindfulness meditation or deep breathing exercises, can significantly aid in preventing migraines. These methods help enhance emotional resilience, ultimately reducing the psychological triggers related to migraine occurrences.
Non-Pharmacological Treatments
In addition to medicinal treatments, non-pharmacological approaches have been shown to effectively alleviate migraine symptoms. Cognitive Behavioral Therapy (CBT) is one popular method that empowers individuals to manage their responses to pain and stress, often leading to a reduction in migraine intensity and frequency.
Biofeedback is another valuable non-invasive treatment option. This mind-body technique teaches individuals to control physiological functions such as heart rate or muscle tension, thus enabling them to recognize and mitigate symptoms before they escalate into full-blown migraines.
Massage therapy has also been shown to help in the management of migraines. Targeted massage techniques can relieve tension in the neck and shoulders, supporting improved posture and circulation. Moreover, it offers a sense of relaxation, which can be beneficial for those burdened by frequent migraines.
Chiropractic adjustments are another alternative treatment that some people find helpful. Through spinal manipulation, chiropractors aim to improve alignment and reduce tension in the neck and shoulders, which can otherwise contribute to headache symptoms, particularly when leaning forward.
Seeking Professional Guidance
For individuals struggling with migraines, seeking professional guidance can provide critical support and insight into effective management strategies. Consulting with a neurologist who specializes in headache disorders can lead to a personalized treatment plan tailored to individual needs and medical history.
Healthcare providers may also suggest working with a registered dietitian to identify potential dietary triggers and create a personalized nutrition plan. Addressing dietary habits not only assists in pain management but can also enhance overall well-being and energy levels.
Moreover, participating in support groups can be immensely beneficial for individuals dealing with chronic migraines. Sharing experiences and coping strategies with others facing similar challenges can foster emotional support and build a sense of community, reducing feelings of isolation.
Finally, regular follow-ups with healthcare professionals ensure ongoing evaluation of treatment efficacy and adjustments to management strategies as needed. Keeping open communication with medical professionals about symptom progress can help in refining treatment plans to achieve optimal results.
5. Eye Care
Understanding Eye Strain and Its Link to Head Pain
Eye strain, or asthenopia, is a common condition that can lead to discomfort and even head pain, especially when leaning forward. When we focus intently on screens or text for prolonged periods, our eyes can become fatigued, causing tension that radiates to the head. This tension often manifests as a dull ache or a sharp pain directly behind the eyes, exacerbated when bending or leaning forward.
Factors contributing to eye strain include improper lighting, excessive screen time, and uncorrected vision problems. When the eyes work harder than usual, they can become overworked and fatigued, leading to head pain that can interfere with daily activities. Implementing measures such as the 20-20-20 rule (taking a 20-second break to look at something 20 feet away every 20 minutes) can significantly reduce strain and discomfort.
Additionally, understanding the ergonomics of your workspace can play a pivotal role in mitigating eye strain. Ensuring the screen is at eye level and using proper lighting can alleviate pressure on the eyes. If discomfort persists despite these adjustments, it may be time to consult an eye care professional for a thorough evaluation and potential corrective measures.
In summary, eye strain is a significant contributor to head pain, particularly in activities that involve leaning forward. By recognizing the symptoms and taking proactive steps, individuals can greatly reduce their discomfort and improve their overall well-being.
Effective Eye Care Practices to Prevent Discomfort
Implementing effective eye care practices is essential for preventing discomfort and alleviating head pain associated with leaning forward. One key practice is maintaining proper hydration. Dehydration can lead to dry eyes and exacerbate feelings of discomfort. Remembering to drink enough water throughout the day can go a long way in keeping your eyes moist and comfortable.
Another important aspect is ensuring that your vision is adequately corrected. Regular eye examinations are crucial for identifying any issues that may worsen eye strain and contribute to headaches. Wearing prescribed glasses or contact lenses, if necessary, will help you see clearly without straining your eyes further.
Adjusting your screen brightness and contrast settings can also help reduce glare and strain on the eyes. Utilizing anti-reflective coatings on glasses and employing blue light filters can significantly lessen the impact of prolonged screen exposure. These small environmental changes can create a conducive atmosphere that supports better eye health.
Incorporating eye exercises into your daily routine can also serve as an excellent preventative measure for eye strain. Simple exercises, such as rolling your eyes or blinking frequently, can aid in relaxing the eye muscles and promoting better focus. Establishing these practices ensures not just comfortable vision but also prevention of associated head pain.
When to Seek Professional Help for Eye-Related Headaches
While many instances of head pain attributed to eye strain can be managed with home remedies and lifestyle adjustments, certain conditions warrant professional attention. If you find that your head pain persists despite your efforts at self-care, consulting an eye care specialist is crucial. They can determine if there is an underlying issue that requires intervention, such as refractive errors or conditions like migraines.
In cases where headaches are accompanied by other symptoms—such as sudden vision changes, light sensitivity, or severe pain—immediate medical attention should be sought. These symptoms could indicate more serious conditions that need addressing to prevent long-term damage and complications.
Additionally, maintaining an open dialogue about your eye health with your healthcare provider can provide insight into your symptoms. Sharing your experiences helps them tailor treatment plans specific to your needs and helps monitor any concerning developments over time.
Overall, understanding when to seek professional help is vital for ensuring there are no additional health concerns contributing to eye-related head pain. Proactive measures, combined with professional oversight, create a comprehensive approach to maintaining good eye health and minimizing discomfort.