The Importance of Thorough Diagnostics

The Role of Accurate Diagnostics in Treatment
Accurate diagnostics are crucial because they guide healthcare providers in developing appropriate treatment plans. Without precise information about a condition, doctors may resort to guesswork, which can lead to ineffective or harmful treatments. A thorough diagnostic process can significantly reduce the chances of misdiagnosis and enhance patient outcomes.
Furthermore, comprehensive diagnostics allow for the identification of comorbid conditions that may complicate treatment. This holistic approach not only addresses the primary ailment but also considers the overall health of the patient. By incorporating all relevant data, healthcare professionals can create more personalized and effective treatment strategies.
Additionally, investing time and resources into thorough diagnostics can potentially save healthcare systems money in the long run. By avoiding the costs associated with repeated hospital visits or ineffective treatments, healthcare providers can enhance resource allocation and improve patient satisfaction.
Challenges in Diagnostic Processes
Despite its importance, the diagnostic process often faces significant challenges. Many healthcare providers are under time constraints that lead to rushed decisions, which may undermine the accuracy of diagnostics. This can result in a lack of comprehensive understanding of patient symptoms and history.
Moreover, the increasing complexity of medical conditions demands sophisticated diagnostic tools and technology, which may not always be available in all healthcare settings. This disparity can create inequities in access to care and affect the quality of treatment received by patients.
Another challenge is the potential for cognitive biases that healthcare providers may face. These biases can skew clinical judgment and impact the decision-making process, ultimately affecting the accuracy of the diagnosis.
The Future of Diagnostics in Healthcare
As technology advances, the future of diagnostics in healthcare looks promising. Innovations such as artificial intelligence and machine learning have the potential to enhance diagnostic accuracy and efficiency. This could lead to earlier detection of conditions and more timely interventions.
Telemedicine is another trend that is reshaping diagnostic practices. Patients can now receive consultations and preliminary evaluations remotely, increasing access to healthcare services, especially for those in underserved areas.
Moreover, personalized medicine, which tailors treatment based on individual genetic profiles, is becoming more prevalent. This approach signifies a shift towards precision diagnostics that can enhance treatment outcomes by focusing on the unique characteristics of each patient.
Case Studies Highlighting the Impact of Root Cause Analysis
Understanding Root Cause Analysis in Healthcare
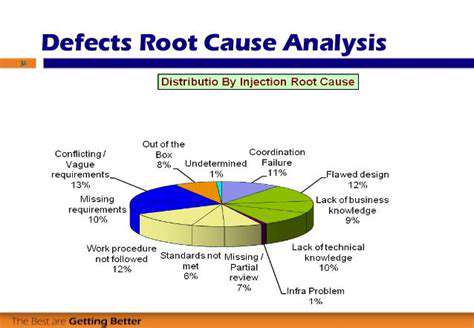
Root cause analysis (RCA) is a systematic approach used to identify the fundamental reasons for problems within healthcare settings. By uncovering the underlying causes of issues, healthcare professionals can implement lasting solutions that improve patient outcomes. Implementing RCA can significantly reduce the likelihood of recurring medical errors. This process involves gathering data, analyzing events, and determining the root causes of adverse events or near misses.
In a healthcare context, RCA often entails investigating incidents such as medication errors, patient falls, or infections. By addressing these root causes, healthcare providers can create safer environments for patients and staff alike. This proactive approach not only enhances safety but also fosters a culture of continuous improvement within institutions. As healthcare becomes increasingly complex, effective RCA is more critical than ever.
An essential aspect of RCA is the involvement of a multidisciplinary team during the analysis process. Engaging diverse perspectives can lead to a more comprehensive understanding of the issues at hand. It also encourages collaboration among healthcare professionals, which is vital for cultivating a safety-oriented culture.
Moreover, continuous monitoring and evaluation of implemented solutions ensure that changes lead to meaningful improvements. Organizations that prioritize RCA are often better equipped to adapt to new challenges in patient care and manage risks effectively.
Case Studies Demonstrating Successful RCA Applications
Numerous case studies illustrate the transformative power of root cause analysis in healthcare. For example, a large hospital implemented RCA after several patients experienced medication errors. Through a thorough examination of protocols and workflows, the team identified gaps in communication and education.
As a result, they developed a comprehensive training program for staff and implemented standardized communication procedures. The outcome was a marked decrease in medication errors, leading to enhanced patient safety and trust in the healthcare system. This case underscores how targeted responses to root causes can yield substantial improvements in healthcare delivery.
Another compelling case study involved a community health center that faced a high rate of patient falls. An RCA team discovered that inadequate environmental safety measures contributed to these incidents. They subsequently redesigned the clinic layout and instituted stricter housekeeping protocols.
The changes led to a significant reduction in patient falls, improving overall patient satisfaction. By addressing the specific root causes instead of merely responding to the symptoms, the center established a more secure environment for its patients.
Challenges in Conducting Root Cause Analysis
Despite its benefits, conducting thorough root cause analysis can present several challenges. One issue is the potential for blame allocation, which can hinder open communication among healthcare staff. Team members may be hesitant to share information out of fear of being held responsible for errors, thereby obstructing the RCA process.
Additionally, inadequate data collection can adversely affect the quality of analysis. If critical information is overlooked or not accurately documented, the RCA may point to misleading conclusions. It is vital for healthcare organizations to cultivate an environment that encourages transparency and honesty to facilitate comprehensive RCA efforts.
Another challenge lies in the implementation of recommended changes post-analysis. Even after identifying root causes, institutions may struggle to enact necessary modifications, often due to resistance to change or lack of resources. Strategic planning and continuous education are essential to overcome these obstacles.
Furthermore, the ever-evolving landscape of healthcare can complicate RCA efforts. Changes in technology, regulations, and patient demographics require adaptability and ongoing assessment to ensure that RCA remains effective and relevant.
Future Directions for Root Cause Analysis in Healthcare
As healthcare continues to evolve, the methodology of root cause analysis is also likely to advance. The integration of technology, such as artificial intelligence and data analytics, can enhance the RCA process by providing deeper insights and identifying patterns in incidents. These tools can help streamline data collection, making RCA more efficient and impactful.
Moreover, fostering a culture of safety and continuous learning within healthcare organizations is critical for the future of RCA. Training staff on the importance of RCA and creating a blame-free environment can significantly enhance the effectiveness of the analysis process.
Collaboration among healthcare entities will also play a vital role in the future of RCA. Sharing best practices, lessons learned, and data can lead to more effective solutions across the industry. An interconnected approach helps achieve a greater understanding of root causes that might affect multiple organizations.
Ultimately, the ongoing commitment to improving patient safety and quality of care requires a sustained focus on root cause analysis. As healthcare systems invest in training, technology, and collaboration, they can expect to see significant advancements in patient outcomes and satisfaction.
Benefits of Holistic Approaches
Understanding the Whole Patient
Identifying root causes of health issues allows healthcare providers to view patients as whole individuals rather than merely a set of symptoms. This approach emphasizes the importance of understanding the complex interplay between biological, psychological, and social factors.
By considering all aspects of a patient’s life, healthcare professionals can tailor treatments to better address their unique circumstances. For instance, the social determinants of health, such as living conditions and access to care, often play a crucial role in health outcomes.
This whole-person view fosters a stronger patient-provider relationship, improving patient satisfaction and adherence to treatment plans. When patients feel understood and valued, they are more likely to engage actively in their healthcare.
Moreover, this perspective encourages collaboration among interdisciplinary teams, enhancing the overall quality of care provided. Physicians, nurses, and therapists can work together more effectively when they share a comprehensive understanding of the patient's situation.
Ultimately, treating the whole patient leads to more sustainable health improvements, as it addresses the root causes of issues rather than just alleviating symptoms.
Improving Diagnostic Accuracy
Root cause analysis is critical in enhancing diagnostic accuracy. By digging deeper into symptoms, healthcare professionals can often uncover underlying conditions that might otherwise go unnoticed.
This is particularly important for chronic illnesses, where early and accurate diagnosis can significantly alter the course of treatment. Identifying the correct root causes can lead to more personalized and effective treatment strategies.
Furthermore, a thorough understanding of root causes can help prevent misdiagnosis and the potential for unnecessary procedures or medications. It minimizes the risk of trial-and-error approaches that are often frustrating for patients and healthcare providers alike.
Incorporating root cause analysis into diagnostic protocols also supports the use of evidence-based practices. Better diagnostics lead to a more targeted and effective application of treatments, increasing the likelihood of successful outcomes.
Healthcare systems that prioritize accurate diagnoses grounded in root cause analysis can significantly improve patient safety and overall healthcare quality.
Encouraging Preventive Care
A key benefit of understanding the root causes of health issues lies in promoting preventive care initiatives. By identifying risk factors related to specific health conditions, healthcare providers can develop targeted strategies that focus on prevention.
For example, if lifestyle factors such as diet, exercise, and stress levels are identified as root causes for chronic illnesses, providers can work with patients on lifestyle modification programs. This proactive approach can significantly reduce the incidence of diseases.
Preventive care not only improves individual health outcomes but also alleviates the burden on healthcare systems by reducing the prevalence of chronic diseases that require costly interventions.
Education is a vital component of preventive care. By informing patients about the root causes of their health issues and ways to mitigate risks, healthcare providers empower them to take charge of their health.
As preventive care efforts flourish, there is the possibility for a cultural shift towards prioritizing health maintenance over reactive treatment, ultimately fostering a healthier population.
Enhancing Treatment Efficacy
Identifying root causes leads to enhanced treatment efficacy by allowing for targeted therapies that address the specific problems at hand rather than just managing symptoms. When treatments are aligned with the underlying issues, patients often experience more rapid and lasting relief.
This specificity not only improves patient outcomes but also increases the efficiency of healthcare resources. Treatments that effectively address root causes can result in reduced hospital admissions and fewer complications, leading to lower costs overall.
Additionally, a focus on root causes can inspire innovation in treatment methodologies. Research into underlying mechanisms can lead to the development of novel therapies that are more effective than existing options.
As healthcare continues to evolve, integrating root cause identification into treatment planning paves the way for precision medicine, where therapies are tailored specifically to the individual's needs based on their unique health profiles.
In summary, enhancing treatment efficacy through understanding root causes is crucial for both patient health and the sustainability of healthcare systems.