you're going about your day when suddenly, a headache strikes with such intensity it feels like being hit by lightning. Now add symptoms like neck stiffness so severe you can't touch your chin to your chest, or perhaps sudden confusion about where you are. These aren't just bad headaches—they're red flags waving frantically for attention. Conditions like meningitis or brain hemorrhages often announce themselves this way, making prompt medical intervention potentially life-saving.Symptoms That Should Trigger Immediate Action
Let's break down the warning signs that separate concerning headaches from true emergencies:
- Visual disturbances: When the world suddenly goes blurry or you see double, your brain might be sounding an alarm
- Neurological symptoms: Weakness on one side, slurred speech, or numbness—these could indicate stroke
- Personality changes: If someone suddenly acts completely out of character during a headache, take notice
I once treated a patient who came in complaining of the worst headache of her life accompanied by an unusual sensitivity to light. What seemed like an extreme migraine turned out to be a subarachnoid hemorrhage. This case underscores why we medical professionals emphasize: when in doubt, get it checked out.
Making the Critical Distinction
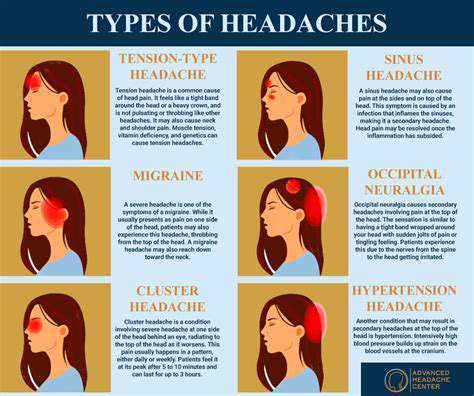
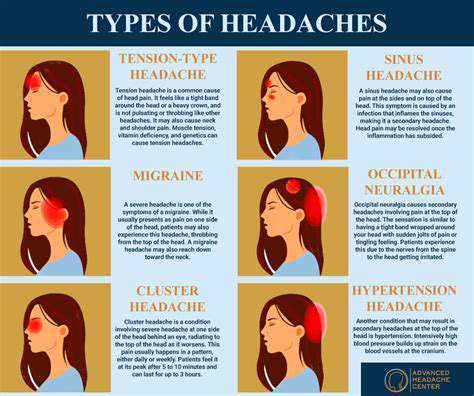
Most headaches follow predictable patterns. Tension headaches feel like a tight band around your head. Migraines often bring nausea and light sensitivity. But emergency headaches? They're different beasts entirely:
| Typical Headache | Emergency Headache |
|---|
| Gradual onset | Instant thunderclap pain |
| Responds to OTC meds | Unaffected by medication |
| No neurological symptoms | Weakness, vision changes present |
The takeaway? If your headache breaks its usual pattern or brings new, worrying symptoms, treat it as suspicious until proven otherwise.
Where to Seek Help
Facing a concerning headache raises an important question: urgent care or ER? Here's a quick guide:
- Urgent care works for:
- Migraines that follow your usual pattern
- Sinus headaches with fever
- Head injuries without loss of consciousness
- ER is mandatory for:
- Headache with stroke symptoms
- After head trauma with confusion
- With high fever and stiff neck
Remember, emergency rooms prioritize life-threatening conditions. If you're questioning whether your headache qualifies, that uncertainty alone suggests ER is the safer choice.
Identifying Headache Severity: A Practical Guide
Mapping Your Pain
Headaches speak in different languages depending on their cause. Location matters tremendously—a band-like tension headache differs sharply from a migraine's one-sided throbbing. I advise patients to mentally map their pain:
- Forehead + cheek pain → Often sinus-related
- Whole-head pressure → Typical tension headache
- One-sided throbbing → Possible migraine
Pain that breaks these patterns warrants extra attention. For instance, occipital (back-of-head) pain with neck stiffness could indicate something more serious.
The Timeline Tells a Story
Duration and progression offer critical clues:
- Short-lived (hours): Probably benign
- Persistent (days): Needs evaluation
- Progressively worse: Red flag
A patient once described his headache as starting mild but steadily increasing over three days. This progression pattern led us to discover elevated intracranial pressure requiring immediate treatment.
Associated Symptoms: The Context Matters
Headaches never exist in isolation. The accompanying symptoms often tell the true story:
Concerning Combinations:
- Headache + fever = Possible infection
- Headache + vomiting without nausea = Potential brain issue
- Headache + seizure = Absolute emergency
These combinations transform an ordinary headache into a medical priority. It's the symptom package, not just the pain itself, that determines urgency.
Personal Factors That Modify Risk
Your medical history acts like a lens, changing how we view any headache:
- History of aneurysms? New headache demands imaging
- Cancer patient? Could indicate metastasis
- Recent head injury? Possible concussion or bleed
Even lifestyle factors matter. A college student pulling all-nighters might just need sleep, while a middle-aged smoker with sudden headache could be having a vascular event.
When Daily Life Becomes Impossible
Functional impairment serves as a crucial severity marker:
- Can you work through it?
- Does light/sound make it unbearable?
- Are you bedridden?
A headache that completely derails normal activity deserves medical attention, even without classic emergency symptoms.
Expert Insights on Headache Management
Why Specialized Knowledge Matters

After years in neurology, I've learned that headache diagnosis is equal parts science and art. Pattern recognition becomes second nature, but so does recognizing when a case defies expectations. The most dangerous mistakes occur when patients or providers dismiss unusual headaches as just another migraine.
Consider these real cases from my practice:
- A migraine patient whose pain always occurred during exercise → Turned out to be a vascular malformation
- Tension headaches that only occurred when bending forward → Revealed a cerebrospinal fluid leak
These examples underscore why professional evaluation matters. What seems obvious often isn't.
Cutting Through the Noise
In our information-saturated world, patients face conflicting advice:
Myth vs Fact:
- Myth: Severity always indicates danger
Fact: Some deadly headaches start mild - Myth: CT scans detect all serious causes
Fact: MRIs often needed for full evaluation
This confusion leads many to either overreact to minor headaches or underestimate dangerous ones. The solution? Establish care with a provider who knows your history. Context transforms vague symptoms into meaningful data.
The Future of Headache Care
Emerging technologies are revolutionizing our approach:
- Wearable devices that track headache patterns
- Telemedicine for rapid specialist consultation
- Advanced imaging that detects subtle abnormalities
Yet despite these advances, the human element remains irreplaceable. Nothing substitutes for a detailed history taken by an experienced clinician. Technology aids, but doesn't replace, clinical judgment.
While differential equations model complex systems in science, headache diagnosis requires its own sophisticated calculus—weighing symptoms, history, and risk factors. The most important equation is simple: unusual headache + new symptoms = prompt medical evaluation. This approach saves lives by catching serious conditions early when treatment is most effective.
Disclaimer: All articles on this site are original, please do not reprint