Diagnosis and Differentiating Status Migrainosus from Other Conditions
Diagnosis of Status Migrainosus
Identifying status migrainosus demands careful clinical evaluation, blending comprehensive patient narratives with detailed neurological assessments. The hallmark lies in recognizing migraine's signature patterns - particularly the cyclical, intense headaches paired with nausea, vomiting, and light/sound sensitivity. Clinicians must document headache chronology meticulously, noting previous attack frequency, duration, and severity. Physical exams should screen for neurological abnormalities that might indicate alternative diagnoses. While aura manifestations don't always accompany status migrainosus, their documentation offers valuable diagnostic insights.
Advanced imaging techniques like CT or MRI become indispensable tools for excluding sinister pathologies that mimic status migrainosus, including cerebral vascular events or intracranial bleeds. These diagnostic modalities serve as critical differentiators, enabling clinicians to distinguish between migraine emergencies and potentially fatal conditions requiring immediate intervention.
Differentiating from Stroke
The clinical distinction between status migrainosus and stroke represents one of neurology's most crucial diagnostic challenges. Both conditions manifest with severe cephalalgia, neurological dysfunction, and possible consciousness alterations. However, three key elements typically separate these entities: symptom evolution timeline, deficit characteristics, and historical patterns.
Cerebrovascular accidents generally announce themselves abruptly, whereas migraine phenomena (including status migrainosus) usually unfold progressively over hours or days. Stroke-related neurological impairments tend to demonstrate precise anatomical localization and rapid progression, contrasting with the more variable, widespread symptoms characteristic of prolonged migraine attacks.
Differentiating from Intracranial Hemorrhage
When confronting patients with thunderclap headaches and neurological compromise, clinicians must maintain high suspicion for intracranial bleeding. This neurosurgical emergency shares several clinical features with status migrainosus, necessitating thorough evaluation of medical background, including trauma history and anticoagulant use. Non-contrast head CT emerges as the diagnostic cornerstone, with hemorrhage detection sensitivity exceeding 95% in acute settings.
Critical differentiators include the typically instantaneous symptom onset in hemorrhagic events versus migraine's gradual progression, along with more pronounced and rapidly worsening focal neurological findings in bleeding scenarios. The presence of meningismus or declining consciousness level should particularly raise concern for hemorrhagic pathology.
Differentiating from Meningitis
Infectious meningeal inflammation creates diagnostic confusion through shared symptoms of severe headache and possible neurological dysfunction. The diagnostic triad of fever, nuchal rigidity, and altered mentation strongly suggests meningeal irritation. When meningitis enters the differential, lumbar puncture becomes mandatory for cerebrospinal fluid analysis, with cell counts, cultures, and PCR testing providing definitive answers.
Migraineurs typically maintain normal body temperature and lack true meningeal signs, though photophobia may simulate light sensitivity seen in meningitis. Careful history-taking remains paramount, as chronic migraine sufferers often recognize their typical headache patterns, while meningitic headaches represent a novel experience for most patients.
Other Differential Diagnoses
The diagnostic landscape broadens further when considering other headache syndromes that might imitate status migrainosus. Giant cell arteritis demands consideration in older patients presenting with new headaches, particularly when accompanied by visual symptoms or jaw claudication. Cluster headaches, while equally debilitating, demonstrate distinct temporal patterns and autonomic features absent in migraine.
Medication overuse headache creates particular diagnostic challenges, as it often develops in chronic migraine patients. A comprehensive medication history proves essential, with particular attention to analgesic consumption patterns. The clinical approach must remain systematic, incorporating detailed history, thorough examination, and judicious use of diagnostic testing to navigate this complex differential.
Just like humans, dogs have a variety of coat types that require different care techniques. Knowing your Dog's Specific Coat Type can significantly affect how you maintain its health and appearance. There are three primary coat types: smooth, wiry, and long-haired. Each type has unique characteristics that dictate grooming frequency and methods. For instance, dogs with long coats often require more frequent brushing to prevent tangles and mats.
Treatment Strategies for Managing Status Migrainosus
Pharmacological Interventions
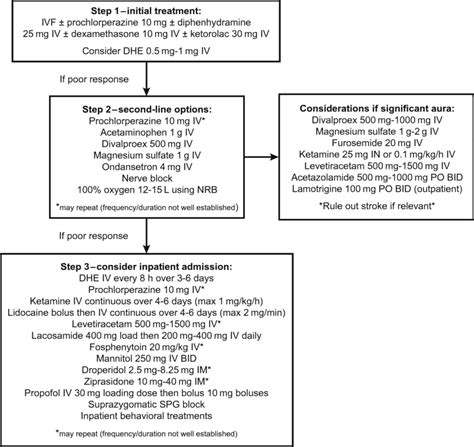
Modern migraine therapeutics employ a multi-pronged pharmacological approach tailored to attack severity and patient response. Acute treatment algorithms typically begin with NSAIDs or migraine-specific agents like triptans, progressing to parenteral options for refractory cases. Preventive pharmacotherapy gains importance for patients experiencing status migrainosus, with options ranging from beta-blockers to newer CGRP antagonists.
Treatment monitoring proves particularly crucial in this population, as medication overuse can paradoxically worsen headache frequency. Regular follow-ups allow for regimen adjustments based on efficacy and side effect profiles, with particular attention to cardiovascular contraindications for certain migraine medications.
Lifestyle Modifications
Non-pharmacological approaches form the foundation of sustainable migraine management, particularly for patients prone to prolonged attacks. Identifying and avoiding personal trigger factors - whether dietary (e.g., aged cheeses, alcohol), environmental (e.g., strong odors, bright lights), or behavioral (e.g., sleep deprivation, stress) - can significantly reduce attack frequency and severity.
Establishing circadian regularity proves especially beneficial, with consistent sleep-wake cycles, meal timing, and hydration patterns helping stabilize neuronal excitability. Many patients find complementary benefit from moderate aerobic exercise, though timing becomes important as exertion during prodromal phases may exacerbate symptoms.
Behavioral Therapies
The biobehavioral dimension of migraine pathophysiology makes psychological interventions valuable adjuncts to medical treatment. Cognitive-behavioral approaches specifically adapted for chronic pain conditions help patients develop coping strategies for attack anticipation and management. Biofeedback training enables enhanced awareness and voluntary modulation of physiological parameters like peripheral vasoconstriction.
Mindfulness-based interventions demonstrate particular efficacy in reducing headache-related disability by altering pain perception and emotional response. These techniques prove especially valuable for patients with comorbid anxiety or depression, which frequently accompany refractory migraine conditions.
Complementary and Alternative Medicine (CAM)
The growing interest in integrative headache medicine has brought several CAM modalities under scientific scrutiny. Acupuncture shows modest efficacy in prevention for some migraineurs, while manual therapies like myofascial release may benefit those with significant musculoskeletal comorbidities. Herbal preparations such as feverfew and butterbur require cautious use due to variable standardization and potential hepatotoxicity.
Patients should always disclose CAM use to their physicians, as interactions with conventional medications can occur, particularly with supplements affecting platelet function or cytochrome P450 metabolism. The placebo response, while substantial in headache disorders, shouldn't replace evidence-based interventions for status migrainosus.
Interventional Procedures
For medication-refractory cases, various procedural interventions may be considered. Nerve blocks targeting the greater occipital nerves can provide temporary relief during acute attacks, while sphenopalatine ganglion blocks show promise for aborting prolonged episodes. Emerging neuromodulation techniques like transcranial magnetic stimulation offer non-invasive alternatives with favorable safety profiles.
Inpatient protocols for status migrainosus often incorporate intravenous dihydroergotamine (DHE) administered with antiemetics, requiring cardiac monitoring due to vasoconstrictive properties. These aggressive interventions necessitate careful patient selection and monitoring in appropriate clinical settings.
Comprehensive Care Models
Optimal management of status migrainosus demands coordinated multidisciplinary care. Headache specialists collaborate with primary providers, pain psychologists, physical therapists, and other specialists to address the condition's multifactorial nature. Digital health tools, including headache tracking applications, enhance treatment personalization through detailed attack pattern documentation.
Support networks, whether formal patient organizations or informal community groups, provide invaluable psychosocial support and practical coping strategies. Educational resources empower patients to recognize warning signs of prolonged attacks early and implement appropriate escalation protocols, potentially preventing full-blown status migrainosus episodes.