Catalog
Common triggers of pain on the side of the head
Identification of accompanying symptoms during migraine attacks
Characteristics of facial pain caused by sinusitis
Features of radiating pain from occipital neuralgia
The relationship between temporomandibular joint disorders and headaches
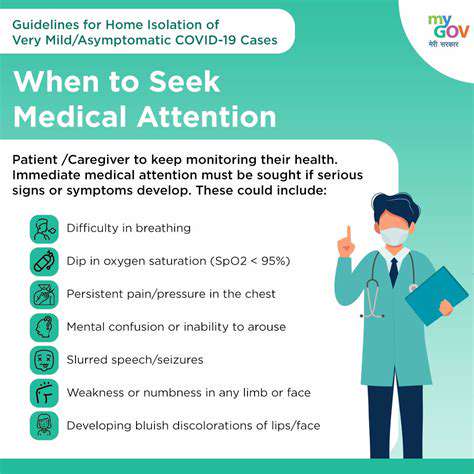
The warning significance of accompanying headache symptoms
The criteria for determining the timing of emergency medical care
Long-term management recommendations for chronic headaches
The practical effectiveness of non-drug therapies
The impact of lifestyle habits on headache frequency
Common triggers of pain on the side of the head

Decoding tension-type headaches
Tension-type headaches are like an invisible tight band wrapped around the head, especially affecting office workers who spend long hours staring at computer screens. Remember the designer Xiao Lin I met at the café last week? He had such a throbbing pain in his temples from working overtime that he couldn't even drink his coffee. According to the American Headache Society, about three-quarters of adults will experience this type of headache at least once in their lifetime. The most cunning aspect of this pain is that it often disguises itself as ordinary fatigue, making people take it lightly.
The disguise of migraines
My cousin is a typical example. Every time she has a migraine attack, not only does the right side of her temple throb, but she also feels nauseous at the slightest whiff of cooking oil from the kitchen. Migraines are experts at diversion tactics; while the pain is located on the side of the head, they come with accomplices like nausea and light sensitivity to cause disruption. A report from the World Health Organization indicated that of every ten migraine sufferers globally, seven are women, which may relate to fluctuations in estrogen.
The confusing tactics of sinusitis
Mr. Wang, a patient I encountered last month in outpatient, is a typical case. He insisted he had migraines, but the CT scan showed it was chronic sinusitis at play. The facial pressure caused by this inflammation often leads people to mistakenly think they are only suffering from a headache.
- Facial swelling and pain can be notably severe in the morning
- A feeling of pressure in the forehead when bending forward
- Increased yellow-green nasal discharge
The lightning strike of occipital neuralgia
This pain feels like someone suddenly stabbing the back of the head with a needle; my neighbor Aunt Li describes it as an electric shock running from her neck to the top of her head. Clinical findings show that about 60% of patients achieve significant relief through nerve block treatment, and combining this with heat therapy and neck stretching yields even better outcomes. It is crucial to differentiate this from cervical spondylosis; do not attempt traction on your own.
The silent protest of the temporomandibular joint
Those who grind their teeth at night should pay special attention! My colleague Xiao Zhang has been suffering from a dull ache in his right temple due to long-term malocclusion. After the dentist fitted him with a bite plate, the frequency of his headaches was reduced by half. Statistics from the American Dental Association indicate that 70% of patients using custom bite plates experienced a decrease of two levels in headache severity. The key is to find a reliable oral specialist.
Warning signals not to be ignored
Dangerous symptom identification guide
A case I treated in the emergency department last week raised concerns: Mr. Liu, 45, thought he had a common headache, but the CT revealed a meningioma. Keep these danger signals in mind:
- Awakening in the early morning with pain accompanied by vomiting
- Sudden blurriness in vision on one side
- Noticeable decline in cognitive function
- Recent history of head trauma
The golden standard for seeking medical care
From my outpatient experience: if the severity of headaches interferes with daily life for more than three days, it's time to head to the hospital. Particularly watch for three first occurrences—first severe headache, first accompanied by fever, first worsening in a specific position. Remember to keep a headache diary:
- Specific location of the pain (a sketch is even better)
- Start and end times of each attack
- Medications taken and their effects
Multifaceted coping strategies
Stepwise medication plan
For occasional headaches, ibuprofen can indeed provide quick relief. However, for long-term patients like Ms. Zhou from our department, who experiences more than eight attacks per month, preventive medication needs consideration. The latest guidelines recommend that topiramate has an efficacy rate of up to 68% in preventing migraines, but be aware of side effects such as numbness in the limbs. When combining medications, I often pair it with magnesium and coenzyme Q10 to enhance effectiveness.
Practical non-drug therapies
Director Li from the acupuncture department shared a typical case: a programmer suffering from superorbital neuralgia due to excessive eye use was able to reduce his medication by 60% through bi-weekly auricular acupressure treatment.  Combined with cognitive behavioral therapy, the effects last longer, especially for tension-type headaches triggered by anxiety.
Combined with cognitive behavioral therapy, the effects last longer, especially for tension-type headaches triggered by anxiety.
Lifestyle transformation plan
My patient group is currently implementing the 3-2-1 plan:
- Micro-movements of the neck three times a day (two minutes each time)
- Aerobic exercise twice a week (heart rate reaching 120 beats/min)
- One hour of digital detox before bed
Wise choices at critical moments
Emergency room vs. outpatient choices
In the early hours of last Wednesday, a 29-year-old fitness trainer came to the emergency department with a thunderclap headache and was diagnosed with subarachnoid hemorrhage. The following situations require calling 120:
- Confusion of consciousness or abnormal behavior
- Stiff neck along with high fever
- Unequal size of pupils on both sides
Management wisdom for chronic headaches
For chronic headaches lasting more than three months, it is recommended to form a medical support team:
- Neurologist (overall management)
- Rehabilitation therapist (posture correction)
- Psychologist (stress management)