Inflammation and Neurological Disorders
The body's immune response relies heavily on inflammation, which presents a nuanced role in neurological conditions. While short-term inflammation aids healing and fights infections, prolonged inflammatory states can wreak havoc on brain tissue, potentially accelerating neurodegenerative processes. Deciphering the complex biological pathways behind persistent inflammation represents a crucial step toward meaningful treatments. This sustained immune activation may trigger neuronal injury, impair synaptic connections, and compromise critical brain operations.
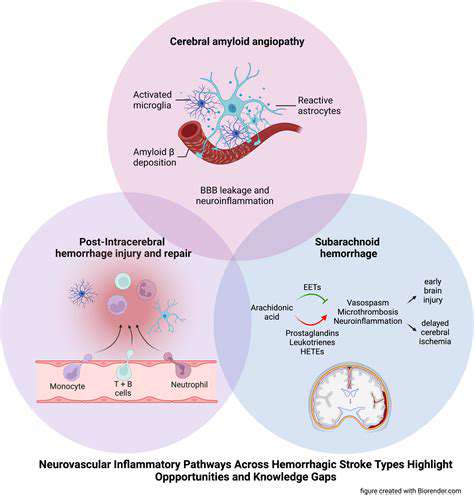
Mounting evidence links chronic inflammation to conditions including Alzheimer's, Parkinson's, and multiple sclerosis. The process involves microglia - the brain's specialized immune cells - which, when constantly activated, release harmful substances that degrade neurons and worsen cognitive and motor symptoms. This neuroinflammatory response has become a focal point for researchers seeking interventions that might interrupt destructive immune cascades.
Cognitive Consequences of Brain Inflammation
Persistent brain inflammation now stands recognized as a major factor in cognitive deterioration. The inflammatory environment disrupts neuronal communication, creating obstacles for information processing. Synaptic plasticity - the brain's adaptability - suffers particularly, leading to challenges with memory formation, learning capacity, and overall mental performance that significantly impact daily functioning.
Research consistently shows that heightened inflammatory markers in cerebrospinal fluid correlate with poorer cognitive test results across diverse groups. Moreover, these inflammatory compounds appear to damage structural integrity in cognition-critical areas like the hippocampus and prefrontal cortex. Individuals with existing cognitive vulnerabilities may experience particularly severe effects from these inflammatory processes.
Neurodegeneration's Inflammatory Roots
Conditions like Alzheimer's and Parkinson's involve progressive neuronal breakdown, with chronic neuroinflammation emerging as a key contributor. The sustained activation of microglia and astrocytes releases neuron-damaging substances that drive disease symptoms forward. This inflammatory component appears deeply intertwined with the pathological hallmarks of these disorders.
Alzheimer's characteristic amyloid plaques and tau tangles may develop partly through inflammatory mechanisms. The complex relationship between immune activation, cellular damage, and abnormal protein accumulation remains an active research frontier. Identifying precise intervention points within these inflammatory pathways could yield breakthrough treatments.
Treatment Horizons and Research Directions
Given inflammation's central role in neurological diseases, developing immune-modulating therapies has become a research priority. Anti-inflammatory approaches that precisely regulate brain immune activity could potentially slow disease progression meaningfully.
Future investigations should pinpoint specific inflammatory molecules and pathways involved in neurodegeneration. Creating therapies that selectively target these elements might revolutionize treatment outcomes. Rigorous clinical trials assessing anti-inflammatory drugs' ability to preserve cognitive function will be essential for validating these approaches.
Neuroinflammation and Migraine Symptoms: A Correlation
Migraine's Inflammatory Component
Central nervous system immune activation has emerged as a significant factor in migraine development. This inflammatory response, triggered by various stimuli, releases substances that directly affect the trigeminal system - migraine's primary pain pathway. Understanding these inflammatory mechanisms could lead to more precise migraine treatments.
Recent studies suggest that low-grade chronic neuroinflammation may heighten pain pathway sensitivity, predisposing individuals to migraine episodes. This sensitization involves receptor changes and neuropeptide release that collectively produce migraine symptoms.
Trigeminal System Vulnerability
The trigeminal system's role in head and face sensation makes it particularly susceptible to inflammatory effects during migraines. Inflammatory mediators can trigger intracranial blood vessel dilation, contributing to migraine's characteristic pulsating pain.
Inflammatory Triggers and Mechanisms
While migraine's inflammatory triggers remain under investigation, several factors appear influential: stress, sleep issues, hormonal changes, environmental elements, and certain foods. These likely initiate inflammatory cascades involving immune cell activation and mediator release.
Genetic factors may also influence individual susceptibility to inflammation-driven migraines. Understanding these variables could enable personalized prevention strategies.
Treatment Innovations on the Horizon
The neuroinflammation-migraine connection opens new therapeutic possibilities. Targeting specific inflammatory pathways might reduce attack frequency and severity. Identifying inflammatory biomarkers could also improve diagnosis and treatment personalization.
Creating an ideal study environment demands thoughtful planning. Natural lighting's importance often gets underestimated - sunlight exposure can dramatically enhance mental alertness. Acoustic considerations matter equally; high-traffic areas rarely support deep concentration. The solution lies in discovering a peaceful space that complements your unique work patterns. Some individuals focus best near windows, while others require more contained spaces. Experimentation remains key to identifying your optimal setup.
Potential Therapeutic Implications: Targeting Neuroinflammation
Innovative Treatment Targets
Discovering new therapeutic targets represents a critical frontier in medical advancement. While current treatments focus on established pathways, unexplored biological mechanisms offer tremendous potential. Novel targets could yield more effective, safer treatments across multiple disease categories. This research requires meticulous investigation of possible side effects, but the clinical benefits could prove transformative. Precision medicines tailored to individual disease profiles might minimize adverse reactions while maximizing therapeutic impact.
Deeper understanding of disease mechanisms remains essential. Mapping molecular and cellular interactions can reveal previously unknown treatment targets. By analyzing these complex networks, researchers may identify disease-specific vulnerabilities that enable highly targeted interventions. This approach proves particularly valuable for complex, heterogeneous conditions where personalized treatment strategies offer the greatest promise.
Enhancing Current Therapies
While pursuing novel targets, improving existing treatments remains equally important. Many current medications face limitations regarding effectiveness, safety, or patient compliance. Optimizing drug formulations, delivery methods, or dosing regimens could significantly boost their therapeutic value. Alternative administration routes or targeted delivery systems might improve efficacy while reducing unwanted effects.
Combining existing therapies with each other or with new agents could create powerful synergistic effects. This combination approach might overcome treatment resistance and enhance overall outcomes, though requires careful evaluation for safety and efficacy. Refining current treatments through innovative combinations could dramatically improve patient quality of life while reducing healthcare system burdens.
Advancing our understanding of drug mechanisms represents another crucial improvement avenue. Detailed knowledge of drug-target interactions enables more precise usage and potentially safer, more effective treatment protocols. This involves comprehensive analysis of how medications interact with biological pathways at molecular levels.