these medications don't work equally well for everyone. Some patients find little relief from these standard options, highlighting the need for personalized solutions.Timing proves crucial with these treatments. Taking medication at the first twinge of migraine symptoms often stops the attack in its tracks. But as hours pass, the window of effectiveness slams shut - delayed treatment means diminished results.
Emerging Therapeutic Strategies
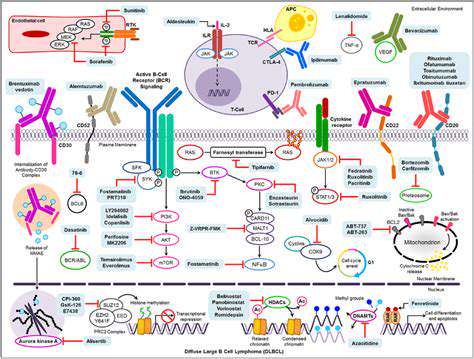
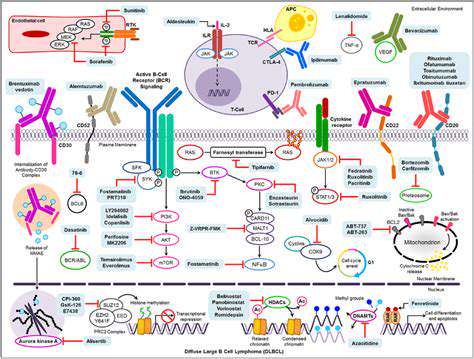
Scientists are racing to develop next-generation migraine treatments that hit different biological targets. The most promising avenues involve blocking specific pain-signaling molecules and calming overactive inflammation pathways. These precision approaches could offer better relief with fewer unpleasant side effects than current options.
The Role of Non-Pharmacological Interventions
While medications take center stage, simple home remedies shouldn't be overlooked. Applying cold packs to throbbing temples, doing light stretches, or practicing deep breathing won't replace prescription drugs, but they can take the edge off symptoms. Many patients report these techniques help them ride out attacks more comfortably when combined with their regular medication.
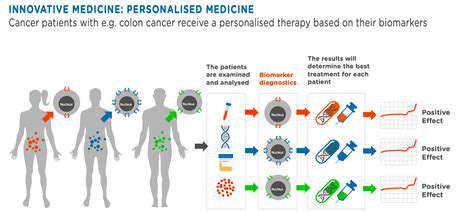
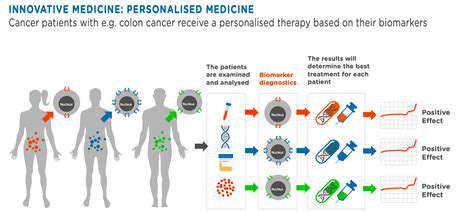
Individualized Treatment Plans
Migraines don't play by the same rules for any two people. What triggers crippling pain for one person might barely register for another. That's why cookie-cutter treatment plans often fail. The solution? Tailoring therapy to each patient's unique migraine patterns, medical history, and lifestyle factors creates the best chance for real relief.
Advances in Diagnostics and Monitoring
Cutting-edge brain scans and nerve activity tests are giving doctors unprecedented views into migraine mechanics. Meanwhile, wearable tech and smartphone apps empower patients to spot their personal triggers and patterns. This two-pronged approach - high-tech diagnostics plus daily self-tracking - is revolutionizing how we understand and manage migraines.
The Importance of Patient Education and Adherence
Knowledge truly is power when battling migraines. Patients who understand their condition - from common triggers to medication timing - gain crucial control over their symptoms. Open doctor-patient communication builds this foundation. Addressing practical hurdles like drug costs and side effects ensures patients can stick with treatments long enough to see results.
Future Directions and Research Priorities
The migraine treatment revolution is just beginning. Researchers are hunting for new drug targets while perfecting diagnostic tools. The most exciting frontier combines medication with neuromodulation techniques and lifestyle changes. This multi-pronged attack could finally give patients the upper hand against debilitating migraine attacks.
Neuromodulation Techniques: Beyond Medications
Non-Pharmacological Approaches
Instead of flooding the body with drugs, neuromodulation tweaks the nervous system's wiring. These high-tech methods use magnets, electricity, or implants to short-circuit migraine pain at its source. Early results suggest they might work when drugs fail, with fewer side effects to boot.
Transcranial Magnetic Stimulation (TMS)
TMS devices deliver magnetic pulses to headache-related brain areas like a precision strike. While scientists are still decoding exactly how it works, the treatment appears to reset overactive pain circuits. Portable TMS units now let patients treat attacks at home - a game-changer for those tired of pill regimens.
Transcranial Direct Current Stimulation (tDCS)
This technique uses mild electrical currents to rebalance brain activity. Early adopters report fewer migraines and better quality of life, though researchers are still fine-tuning the ideal settings. The non-invasive approach makes it appealing for long-term use.
Electrical Nerve Stimulation
Zapping specific nerves in the head or neck shows promise for short-circuiting migraine pain. Different devices target various nerve bundles, with some patients reporting dramatic relief. As technology improves, these treatments could become go-to options for drug-resistant cases.
Vagal Nerve Stimulation
Originally developed for epilepsy, vagus nerve stimulators are getting a second look for migraines. The implanted devices send regular pulses to this major nerve, potentially preventing attacks before they start. While invasive, they offer hope for those with daily debilitating migraines.
Biofeedback and Relaxation Techniques
Biofeedback machines turn the body's stress signals into visible data, teaching patients to short-circuit tension before it triggers migraines. Combined with relaxation practices, these methods put prevention in patients' hands - literally. Many find they need less medication after mastering these techniques.
Deep Brain Stimulation (DBS)
Reserved for extreme cases, DBS involves brain surgery to implant stimulation electrodes. While still experimental for migraines, it's shown remarkable results for other chronic pain conditions. As technology miniaturizes, this last-resort option may become safer and more accessible.
Creating a calm environment can significantly reduce stress levels in individuals. The connection between serene surroundings and migraine prevention is stronger than many realize. Quiet, organized spaces give overstimulated nervous systems the break they need to avoid triggering attacks.
Disclaimer: All articles on this site are original, please do not reprint