Pinpointing personal migraine triggers forms the foundation of any successful prevention plan. While triggers vary widely—from emotional stress and dietary choices to sleep irregularities and weather shifts—recognizing these catalysts allows patients and doctors to craft tailored interventions.
Types of Migraine Preventative Medications
The medical arsenal against migraines includes diverse preventive options, each with unique biological targets and possible adverse effects. Standard categories encompass beta-adrenergic blockers, tricyclic antidepressants, antiepileptic drugs, and the groundbreaking CGRP antagonists. Since these medications influence different migraine pathways, consulting a specialist becomes imperative to match the treatment to the patient's specific condition.
CGRP inhibitors represent a revolutionary approach, directly neutralizing calcitonin gene-related peptide—a key player in migraine pathology. Their precision in thwarting migraine episodes has positioned them as game-changers in neurological therapeutics.
Lifestyle Modifications for Prevention
While pharmaceuticals are vital, behavioral adjustments constitute an equally critical prevention pillar. Establishing circadian rhythm consistency, mastering stress-reduction methods like mindfulness meditation, and consuming a nutrient-dense diet with particular attention to magnesium and riboflavin intake can collectively reduce migraine susceptibility.
Physical activity, even light aerobic exercise three times weekly, demonstrates protective effects against migraine recurrence. Additionally, maintaining optimal hydration and identifying then avoiding personal trigger factors—whether aged cheeses, strong perfumes, or barometric pressure changes—can substantially decrease attack likelihood.
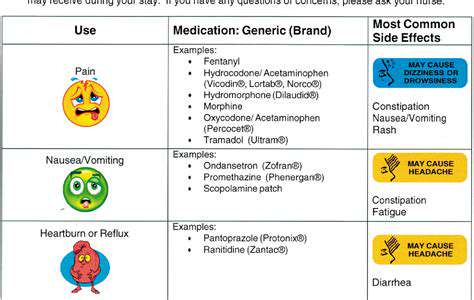
Potential Side Effects and Considerations
Like all pharmacotherapies, migraine preventives carry possible undesirable effects that differ by drug class and individual tolerance. Commonly reported issues include gastrointestinal discomfort, vertigo, daytime drowsiness, and cardiovascular parameter fluctuations. Patients should maintain open dialogue with prescribers about any concerning symptoms and understand that side effects often diminish with continued use.
It's particularly important to recognize that most preventive agents require 6-8 weeks to reach full efficacy, and some individuals paradoxically experience initial symptom exacerbation. This transitional phase shouldn't prompt premature discontinuation without medical consultation.
Medication Interactions and Monitoring
Transparent medication reconciliation is non-negotiable—healthcare teams need complete lists of all prescription drugs, OTC products, nutraceuticals, and botanical supplements the patient uses. Undisclosed drug combinations can dangerously alter preventive medication pharmacokinetics or precipitate adverse reactions. Scheduled therapeutic drug monitoring ensures optimal dosing and timely regimen adjustments.
Particular vigilance applies to cardiovascular parameters with certain preventives, necessitating periodic ECGs or bloodwork. Neurologists typically employ a treat-to-target strategy, methodically escalating therapy until achieving adequate migraine control.
Patient Education and Adherence
Successful prophylaxis hinges on patient literacy regarding their treatment rationale and the consequences of inconsistent use. Empowered patients who track headache patterns, voice concerns promptly, and implement recommended lifestyle changes experience superior outcomes compared to passive recipients of care.
Comprehensive migraine education should cover prodrome recognition, acute rescue medication strategies, and non-pharmacological pain modulation techniques to create a robust self-management framework.
When to Seek Professional Help
Migraines warrant specialist evaluation when exceeding 4 monthly episodes, causing prolonged disability, or resisting first-line interventions. Timely neurology referral becomes crucial for patients experiencing aura symptoms, medication overuse headaches, or concerning neurological findings during attacks.
Early specialist involvement can prevent chronic migraine transformation and identify secondary headache disorders masquerading as migraines, ensuring appropriate diagnostic workup and targeted therapy.