Tension Headaches: The Most Common Type of Head Pain
Tension Headaches: A Closer Look
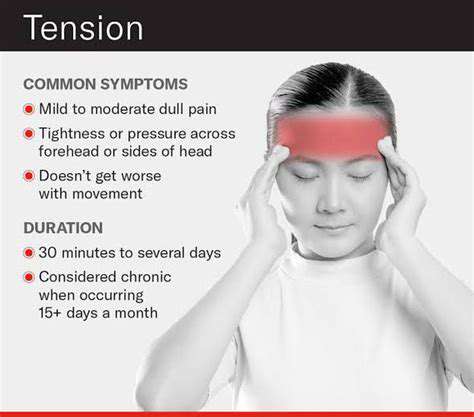
Tension headaches are the most prevalent form of headache, affecting millions of people worldwide. This type of headache is characterized by a dull, aching pain on both sides of the head. They can be triggered by stress, poor posture, or lack of sleep, making them very common in our fast-paced lives. Tension headaches can last from 30 minutes to several days, and while they are not usually debilitating, they can significantly impact daily activities. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are commonly used to alleviate this type of pain.
Triggers and Symptoms of Tension Headaches
Identifying triggers is crucial in managing tension headaches effectively. Common triggers include stress, anxiety, and muscle tension in the neck and shoulders. Additional symptoms may include sensitivity to light or sound, but these are generally less severe than those associated with migraines. Recognizing the early signs can help individuals take measures to mitigate the pain before it escalates. In many cases, tension headaches can be preventable through lifestyle changes and relaxation techniques.
Effective Treatments and Management Strategies
For those suffering from frequent tension headaches, various treatment options are available. Non-prescription medications provide quick relief for mild to moderate headaches. However, for chronic cases, doctors may recommend prescription medications or physical therapy to address underlying issues. Additionally, practicing relaxation techniques such as deep breathing or yoga can be beneficial. Maintaining a regular sleep schedule and staying hydrated can also play a vital role in prevention.
When to Seek Professional Help
While tension headaches can often be managed at home, it’s essential to consult a healthcare professional if headaches become more frequent or severe. Persistent or debilitating headaches might indicate a more serious underlying condition, requiring medical attention. Doctors can provide a thorough evaluation and recommend appropriate treatment plans tailored to individual needs. Early intervention can lead to better management and improvement in quality of life. Understanding when to seek help is vital in achieving long-term relief.
Migraines: More Than Just a Headache
Migraine Symptoms and Triggers
Migraines are often characterized by intense, pulsing pain, usually on one side of the head. Many sufferers also experience accompanying symptoms such as nausea, vomiting, and sensitivity to light and sound.
Common triggers for migraines can vary significantly from person to person. Common factors include hormonal changes, specific foods, stress, sleep disturbances, and environmental factors like bright lights or strong odors. Understanding personal triggers is key to managing migraines effectively.
In addition to these triggers, some individuals may experience auras—visual or sensory disturbances—before the onset of a migraine. Auras can manifest as flashes of light, blind spots, or tingling sensations in the extremities.
Treatment Options for Migraines
Managing migraines often involves a combination of lifestyle changes, preventive medications, and acute treatments. Over-the-counter pain relievers like ibuprofen or acetaminophen can sometimes alleviate mild migraine pain.
For more severe or chronic migraines, healthcare providers may prescribe medications specifically designed to abort attacks or prevent them altogether. These can include triptans, ergots, or newer medications such as CGRP inhibitors.
Non-pharmacological treatments like cognitive-behavioral therapy, biofeedback, and acupuncture have also shown promise in helping some individuals reduce the frequency and severity of migraine attacks.
Lifestyle Adjustments for Managing Migraines
Incorporating lifestyle adjustments can play a significant role in migraine management. Maintaining a regular sleep schedule, staying hydrated, and eating balanced meals can help prevent migraine occurrences.
Stress management techniques, including mindfulness meditation and relaxation exercises, can be beneficial to reduce the likelihood of stress-induced migraines. Finding effective coping strategies is essential for individuals with chronic migraines.
Lastly, keeping a migraine diary can be a practical tool for tracking symptoms, triggers, and potential prevention strategies. This information can be invaluable for healthcare providers in tailoring the most effective treatment plan.
Cervical Spondylosis: Age-Related Wear and Tear
Cervical Spondylosis: Understanding the Condition
Cervical spondylosis, often referred to as cervical osteoarthritis, is a common age-related condition that affects the cervical spine. As individuals age, the intervertebral discs and vertebrae in the neck undergo natural wear and tear. This degeneration can lead to stiffness, pain, and a reduced range of motion.
The condition is primarily caused by the loss of hydration in the discs and the formation of bone spurs, which can compress nerves and lead to additional discomfort. Symptoms often vary among individuals, with some experiencing chronic pain while others may have intermittent episodes of discomfort.
Diagnosis usually involves a thorough physical examination, along with imaging tests such as X-rays or MRIs to assess the extent of degeneration and rule out other potential causes of neck pain.
It's important to note that cervical spondylosis is a progressive condition, meaning that symptoms can worsen over time. Therefore, early intervention and lifestyle modifications can be crucial in managing pain and maintaining mobility.
Common treatment options include physical therapy, pain medications, and in some severe cases, surgical intervention may be necessary to relieve nerve compression or improve spinal stability.
Managing Symptoms of Cervical Spondylosis
Managing the symptoms of cervical spondylosis often involves a combination of medical treatment and self-care strategies. Physical therapy is frequently recommended to strengthen the neck muscles and improve posture, which can help alleviate some of the stress on the cervical spine.
Additionally, patients are encouraged to engage in regular low-impact exercise, such as walking or swimming, to maintain overall fitness without placing undue strain on the neck. Stretching and range-of-motion exercises can also be beneficial in promoting flexibility and reducing stiffness.
Applying heat or cold to the neck can provide temporary relief from pain and inflammation. Heat therapy can relax tense muscles, while cold therapy can numb sharp pain and reduce swelling.
Over-the-counter pain relief medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), can be effective for managing pain associated with cervical spondylosis. In cases of severe pain, a healthcare provider may prescribe stronger medications or suggest alternative therapies, such as acupuncture or chiropractic care.
Lastly, patients should maintain a healthy lifestyle, including proper hydration, nutrition, and adequate sleep, all of which play a crucial role in overall musculoskeletal health and can help mitigate the effects of cervical spondylosis.
Whiplash Injuries: More Than Just a Sudden Jolt
Understanding Whiplash Injuries
Whiplash injuries occur when the head is suddenly jerked forward and then back, straining the muscles and ligaments in the neck. This can often happen during car accidents or sports activities, where an abrupt impact is involved.
The symptoms can vary widely, ranging from neck pain and stiffness to headaches and tingling in the arms. In some cases, individuals may also experience dizziness and fatigue. Understanding the mechanics of a whiplash injury is essential to appreciate the severity and potential long-term effects.
After an initial injury, it’s not uncommon for symptoms to potentially worsen over the days following the event. The delayed onset can often leave individuals confused about the source of their pain.
Seeking prompt medical evaluation can help in the diagnosis and treatment of whiplash injuries, allowing for appropriate interventions to begin sooner.
Symptoms of Whiplash Injuries
Whiplash can manifest a variety of symptoms that may not appear immediately after the initial injury. Commonly reported symptoms include neck pain, reduced range of motion, and discomfort when moving the head.
Headaches often accompany neck pain and can range from mild to debilitating in nature. Patients may also experience tension or soreness in the shoulders and upper back.
Other symptoms can include fatigue, sleep disturbances, and even changes in memory or mood. It’s important to keep in mind that these symptoms can evolve over time, making it essential for individuals to monitor their health following a whiplash injury.
Effective management strategies can help alleviate symptoms and allow for a quicker return to normal activities.
Preventative Measures and Treatment Options
Prevention of whiplash injuries begins with proactive measures such as proper seating and head restraint use in vehicles. Utilizing seatbelts and ensuring that vehicles are equipped with safe features can significantly mitigate the risk of injury during an accident.
In terms of treatment, rest and ice applications can help reduce inflammation and pain in the initial stages. Physical therapy is often recommended to strengthen the neck muscles, enhance flexibility, and restore function.
Medications such as pain relievers or muscle relaxants may also be prescribed to manage discomfort effectively. In more severe cases, interventions may include chiropractic care or acupuncture as complementary therapies.
Long-term management might also involve lifestyle changes, ergonomic considerations at work, and ongoing exercises to maintain neck health. Prioritizing these aspects can greatly influence recovery and overall well-being.