A Common Headache DisorderMigraine represents a widespread neurological condition marked by recurring, often severe headaches. These painful episodes typically come with additional symptoms like nausea, vomiting, and extreme sensitivity to light and noise. Migraine attacks can dramatically disrupt normal activities, affecting job performance, academic work, and social interactions.
The underlying biological mechanisms driving migraines involve complex interactions that researchers continue to study. Multiple factors appear to contribute including genetic susceptibility, environmental triggers, hormonal changes, and psychological stress.
Key Symptoms of IIH
IIH symptoms vary considerably among patients, but commonly include persistent, pounding headaches frequently centered around the temples or back of the head. These headaches often intensify with actions like coughing, sneezing, or physical exertion.
Visual disturbances represent another hallmark symptom, including double vision, blurred sight, or temporary vision loss. Ophthalmologists may detect papilledema (optic nerve swelling) during comprehensive eye examinations.
Key Symptoms of Migraine
Migraine headaches typically feature throbbing or pulsating pain, usually concentrated on one side of the head. The discomfort ranges from moderate to severe and commonly persists for several hours or multiple days.
Associated symptoms frequently include nausea, vomiting, and extreme sensitivity to light and sound (photophobia and phonophobia). These accompanying issues often make migraines particularly disabling.
Comparing IIH and Migraine Headaches
While both conditions cause headaches, they differ substantially in their origins and associated symptoms. IIH stems from elevated intracranial pressure, whereas migraines result from various triggers. The presence of vision problems, papilledema, and exertion-aggravated headaches strongly indicates IIH rather than migraine. Accurate diagnosis proves essential for proper treatment.
Diagnosis and Treatment Approaches
Diagnosing IIH requires comprehensive evaluation by neurologists or ophthalmologists, including detailed medical history, physical examination, neurological testing, and possibly MRI or CT scans. Precise diagnosis ensures appropriate treatment, as IIH and migraine require different therapeutic approaches.
IIH treatment focuses on reducing intracranial pressure, while migraine management aims to control pain and prevent future episodes. Treatment plans may incorporate medications, lifestyle adjustments, or other therapies tailored to individual needs.
Prevention and Management Strategies
While complete IIH prevention remains challenging due to uncertain causes, maintaining healthy habits supports overall wellbeing and may reduce risk factors. These include balanced nutrition, regular physical activity, and stress reduction techniques. For migraine sufferers, identifying and avoiding personal triggers like stress, caffeine withdrawal, and specific foods can substantially decrease attack frequency and severity.
Regular follow-up visits with healthcare providers help monitor conditions and adjust treatment plans as needed, particularly important for both IIH and migraine patients.
Diagnostic Challenges and Overlap
Differentiating Symptoms
A major diagnostic challenge involves symptom overlap between conditions. Many disorders share similar presentations, complicating accurate diagnosis. This overlap can result in misdiagnosis or treatment delays, potentially harming patients. For instance, fatigue may signal anything from minor viral infections to serious conditions like anemia or depression.
Meticulous attention to detail, comprehensive history-taking, and thorough physical examination help distinguish between possible causes. This systematic approach eliminates less likely possibilities, focusing the diagnostic process on probable conditions. Appropriate diagnostic testing further aids accurate identification.
Confounding Variables
Multiple factors can complicate diagnosis by influencing symptom interpretation. These include pre-existing conditions, lifestyle factors, environmental exposures, and patient symptom perception. Accounting for these variables proves essential for accurate diagnosis.
For example, hypertensive patients may display symptoms mimicking other conditions, potentially delaying correct diagnosis. Complete medical history review, including potential confounding factors, remains critical for proper diagnosis.
Limited Diagnostic Tools
Sometimes available diagnostic methods cannot definitively identify a condition's cause. This limitation may stem from condition complexity, lack of specific tests, or assessment difficulties. Complex cases may require multidisciplinary specialist involvement.
Advanced imaging and lab tests don't always provide definitive answers. Additional investigation like genetic testing or specialized procedures may become necessary in challenging cases.
Subtle and Gradual Onset
Some conditions develop gradually with subtle symptoms, complicating early diagnosis. Patients or providers may dismiss early signs as insignificant, delaying proper intervention. This insidious onset obscures symptom origins, making initial symptom timing difficult to pinpoint.
Early detection proves crucial for effective management. Regular health checkups and prompt attention to unusual changes improve chances for timely intervention and better outcomes.
Diagnostic Overlap with Other Conditions
Numerous medical conditions share similar symptoms, creating diagnostic confusion. Careful consideration of medical history, physical findings, and test results helps differentiate between conditions.
The Role of Patient History
Detailed patient history plays a pivotal diagnostic role. Gathering comprehensive information about symptoms, medical background, lifestyle, and family history helps identify potential causes while excluding unlikely conditions. Patient symptom descriptions provide valuable insights.
Thorough history facilitates both accurate diagnosis and personalized treatment planning. Properly assessing the patient's subjective experience remains essential for comprehensive diagnosis.
Treatment Approaches and Management Strategies
Pharmacological Interventions
Medications form a foundation for treating many conditions by targeting specific biological pathways or symptoms. Careful attention to potential side effects and drug interactions remains essential, as does monitoring patient responses. Pharmacotherapy often helps manage chronic conditions, improving symptom control and quality of life.
Different conditions require different medications - some target inflammation while others affect neurotransmitter levels. Selecting appropriate medications demands thorough understanding of patient history, current health status, and potential risks.
Non-Pharmacological Therapies
Non-drug therapies provide valuable alternatives or complements to medications. These approaches emphasize lifestyle and behavioral changes to enhance health. Examples include dietary modifications, exercise regimens, and stress reduction techniques. Such methods can effectively manage certain conditions while reducing medication dependence.
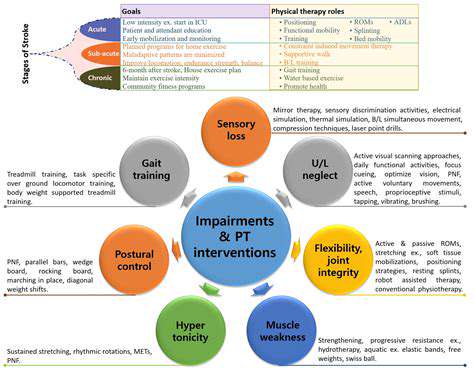
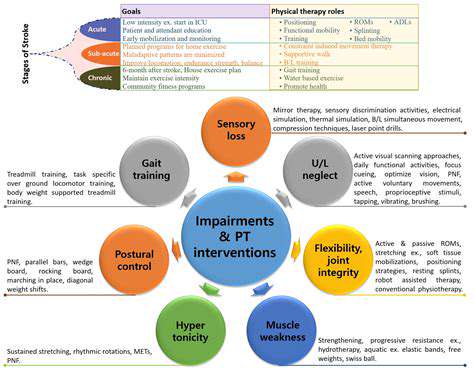
Physical therapy, occupational therapy, and counseling represent additional non-pharmacological options. These approaches address physical limitations, improve functional abilities, and provide psychological support respectively, helping restore function and improve life quality.
Lifestyle Modifications
Lifestyle changes prove crucial for managing many health conditions and promoting wellbeing. These include adopting healthier eating patterns, regular physical activity, sufficient sleep, and stress management. Implementing these changes can dramatically improve health outcomes and reduce chronic disease risks.
Dietary adjustments significantly impact conditions like diabetes and heart disease. Regular exercise benefits both physical health and mental wellbeing. While adopting lasting lifestyle changes requires time and commitment, the long-term advantages typically outweigh initial challenges.
Complementary and Alternative Medicine (CAM)
Complementary and alternative therapies gain increasing recognition for potential health benefits. These approaches often complement conventional treatments to enhance effectiveness. CAM examples include acupuncture, herbal remedies, and mindfulness practices.
Patient Education and Support
Patient education and support significantly influence treatment success. Teaching patients about their condition, treatment options, and potential side effects empowers active care participation. This enables informed decision-making and effective condition management.
Support groups and counseling services connect individuals facing similar challenges, providing emotional support, practical advice, and community. Strong support networks improve treatment adherence and overall wellbeing.
Monitoring and Evaluation
Regular monitoring and assessment form essential treatment components. This process tracks progress, evaluates intervention effectiveness, and adjusts treatment plans as needed. Close monitoring helps identify potential complications or adverse reactions early.
Follow-up visits, lab tests, and symptom assessments all contribute to monitoring. These evaluations help ensure continued treatment effectiveness and safety while addressing evolving patient needs.
Disclaimer: All articles on this site are original, please do not reprint