symptoms emerging predictably after migraine attacks and gradually improving over time. They may order imaging studies to rule out more serious neurological conditions, especially when symptoms appear for the first time in older patients.The challenge lies in distinguishing postdrome from medication overuse headaches or rebound phenomena, which can create similar lingering symptoms. This distinction becomes crucial because treatment approaches differ significantly. A detailed headache diary tracking symptoms before, during, and after attacks often provides the clearest diagnostic picture.
Treatment Strategies for Managing Postdrome
Managing postdrome symptoms requires a tailored approach. For the persistent headache component, some patients find relief with gentle non-steroidal anti-inflammatories, while others benefit more from hydration and electrolyte replacement. Cognitive symptoms often respond best to strategic rest - short, scheduled naps rather than prolonged bed rest that can disrupt nighttime sleep.
Many patients report success with sensory modulation techniques during this phase. Wearing blue-light blocking glasses helps with light sensitivity, while noise-canceling headphones can make environments with unavoidable sound more tolerable. Perhaps most importantly, patients learn to honor their body's need for recovery time rather than pushing through symptoms.
Lifestyle Modifications and Prevention
Preventing severe postdrome starts with migraine prevention. Consistent sleep patterns prove crucial - both in terms of duration and timing. Many patients discover their migraines become more frequent when they deviate from their usual sleep schedule, even on weekends. Dietary modifications often help too, with many patients benefiting from regular meal times and careful attention to hydration.
Stress management techniques show particular promise for reducing both migraine frequency and postdrome severity. Mindfulness practices, when used consistently, can help patients develop greater awareness of early warning signs. Some patients find biofeedback helpful for recognizing and controlling physiological stress responses that may contribute to migraine cycles.
Common Symptoms of the Migraine Postdrome
Early Warning Signs
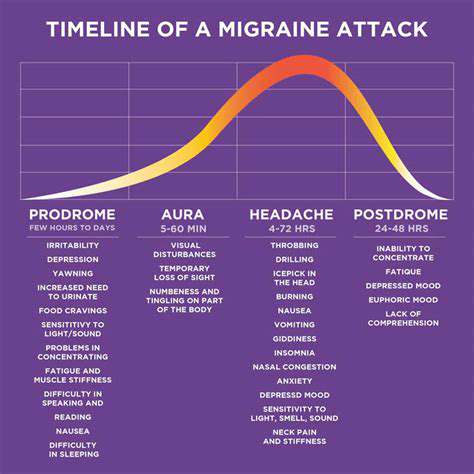
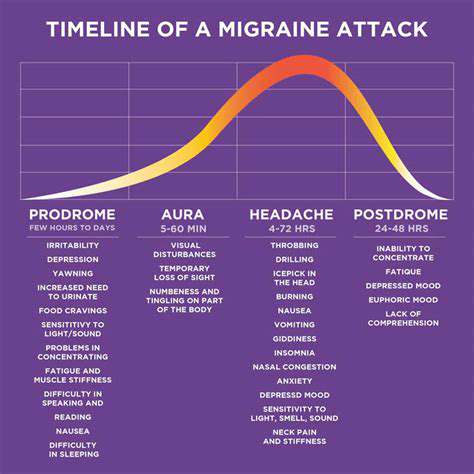
Prodromal symptoms serve as the body's early alert system, though many patients don't recognize them until they've experienced several migraine cycles. These subtle changes can include unusual food cravings - particularly for sweet or salty foods - or sudden bouts of yawning that seem disproportionate to actual tiredness. Some patients report increased thirst or urinary frequency in the days before an attack.
Learning to recognize these signals can provide a critical window for early intervention. Patients who identify their prodrome can sometimes use preventive measures like hydration, stress reduction, or early medication to potentially lessen the severity of the coming attack and subsequent postdrome.
Headache Characteristics
While the severe throbbing pain typically subsides during postdrome, many patients experience residual headache symptoms. This often manifests as a dull, constant pressure rather than sharp pain. The location may shift from the original migraine site, sometimes spreading to involve the entire head or concentrating at the base of the skull.
What makes postdrome headaches particularly frustrating is their unpredictable response to treatment. Medications that work well for acute migraine attacks often prove less effective for these lingering symptoms, prompting the need for alternative management strategies.
Nausea and Digestive Symptoms
Gastrointestinal disturbances can persist well into the postdrome phase. Some patients describe a lingering queasiness that makes eating unappealing, while others experience specific food aversions - often to smells or flavors they normally enjoy. This can create nutritional challenges during recovery.
Hydration strategies become particularly important during this phase. Many patients find small, frequent sips of electrolyte solutions more tolerable than large volumes of plain water. Ginger-based remedies or peppermint tea sometimes help settle persistent nausea when traditional antiemetics aren't effective.
Cognitive and Emotional Symptoms
The cognitive impact of postdrome often surprises patients and their families. Many describe a brain fog that makes concentration difficult and memory retrieval sluggish. This can manifest as forgetting where they placed items, struggling to follow conversations, or making uncharacteristic errors in routine tasks.
Emotionally, patients may experience mood swings ranging from irritability to tearfulness. This emotional lability often stems from physiological changes rather than psychological distress, though the distinction can be difficult to recognize in the moment. Understanding these symptoms as part of the biological recovery process helps patients and families respond with appropriate patience and support.
Managing the Postdrome: A Multifaceted Approach
Understanding Recovery Needs
Postdrome management begins with recognizing it as a legitimate phase of recovery rather than simply feeling tired. The body has undergone significant neurological and vascular changes during the migraine attack, and the postdrome represents its attempt to restore equilibrium. Pushing through this phase often prolongs recovery, while appropriate self-care can shorten it.
Symptom-Specific Strategies
Different symptoms require tailored approaches. For cognitive symptoms, patients report success with mental downtime - avoiding complex decision-making and cognitively demanding tasks when possible. Physical symptoms often respond best to gentle movement rather than complete rest - short walks or light stretching can improve circulation without overtaxing the recovering system.
Sensory symptoms frequently benefit from environmental modifications. Dimming lights, reducing screen time, and creating quiet spaces can make the recovery period more comfortable. Some patients find acupressure or gentle massage helpful for residual headache symptoms.
Nutritional Support
The postdrome phase often creates unique nutritional challenges. Many patients experience decreased appetite but increased nutritional needs during recovery. Small, nutrient-dense meals and snacks can help bridge this gap. Foods rich in magnesium and B vitamins may be particularly beneficial, though individual responses vary.
Hydration remains crucial, especially if the migraine attack included vomiting or decreased fluid intake. Electrolyte solutions can help restore balance more effectively than plain water for some patients. Monitoring urine color provides a simple way to assess hydration status - pale yellow indicates adequate hydration.
Gradual Return to Activity
Resuming normal activities requires careful pacing. Many patients benefit from a phased approach - beginning with light household tasks before attempting work responsibilities. Cognitive tasks should similarly progress from simple to complex. This gradual approach helps prevent symptom exacerbation while rebuilding stamina.
Communication with employers, teachers, or family members can facilitate this transition. Explaining that recovery continues after pain subsides helps set realistic expectations. Some patients find written checklists helpful for tracking their progress through recovery milestones.
Just as careful preparation leads to successful furniture restoration, attentive self-care during postdrome promotes optimal recovery.
Seeking Professional Help and Support

When to Consult a Specialist
While many patients manage occasional migraines independently, professional guidance becomes valuable when postdrome symptoms significantly impact quality of life or work performance. Warning signs include postdrome phases lasting more than three days, increasing frequency of attacks, or symptoms that worsen rather than improve over time.
Specialized headache clinics offer the most comprehensive care, combining neurological expertise with multidisciplinary support. These centers can provide advanced treatment options and help identify subtle patterns that might escape notice in general practice.
Building a Treatment Partnership
Effective migraine management requires collaboration between patient and provider. Keeping detailed records of attacks, symptoms, and responses to various treatments provides the foundation for personalized care. Many patients find smartphone apps or dedicated headache diaries helpful for tracking this information systematically.
Treatment plans should evolve based on ongoing assessment. What works during one phase of life may become less effective over time. Regular follow-ups allow for necessary adjustments and ensure emerging research findings get incorporated into care plans.
Exploring Comprehensive Approaches
Modern migraine management extends beyond medication. Many clinics now offer integrated services including nutritional counseling, physical therapy, and behavioral health support. These complementary approaches can address various aspects of the migraine cycle, including postdrome symptoms.
Behavioral interventions like cognitive behavioral therapy show particular promise for helping patients develop coping strategies and modify thought patterns that might inadvertently exacerbate symptoms. Biofeedback training can enhance awareness of physiological stress responses, providing tools for better self-regulation.
Navigating Workplace Accommodations
For patients whose postdrome symptoms interfere with work performance, professional support can help secure appropriate accommodations. Neurologists can provide documentation supporting needs like flexible scheduling during recovery periods, modified lighting in workspaces, or permission to use noise-reducing headphones.
Human resources professionals can advise on legal protections and workplace policies. Many patients qualify for intermittent leave under laws like the Americans with Disabilities Act, though specific provisions vary by location and employment situation.
Connecting with Support Networks
Patient support groups offer unique benefits that complement clinical care. Sharing experiences with others who understand the challenges of migraine can reduce feelings of isolation and provide practical coping tips. Many organizations now offer virtual support options, making these resources accessible regardless of location.
Family education represents another crucial component of support. Helping loved ones understand postdrome symptoms fosters patience and appropriate expectations during recovery periods. Many clinics offer educational materials specifically designed for family members.
Disclaimer: All articles on this site are original, please do not reprint