What Causes Vestibular Disorders?
Understanding the Inner Ear's Role
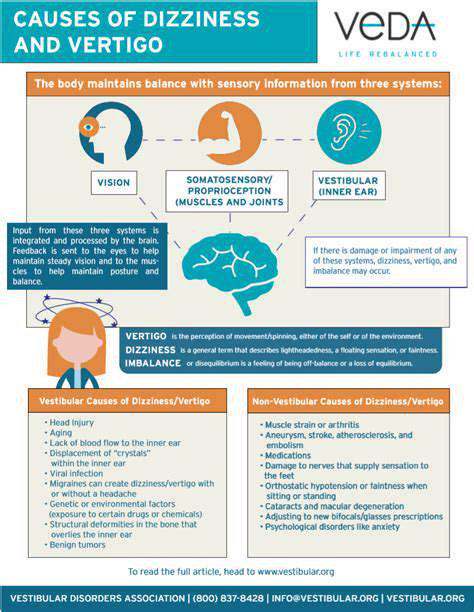
The inner ear is a crucial component of the vestibular system, which helps maintain balance and spatial orientation. Any disruption in this intricate structure can lead to vestibular disorders. This area contains the semicircular canals and otolith organs, which detect rotational and linear movements. When these sensors fail, they can cause symptoms such as dizziness, vertigo, and balance problems, significantly impacting daily life.
The semicircular canals are fluid-filled structures that respond to head rotation, while the otolith organs detect gravity and acceleration. If either of these components is affected by infections, physical trauma, or degenerative diseases, it can lead to dysfunctional signals being sent to the brain. This miscommunication can be disorienting and is a primary factor in many vestibular disorders.
Common conditions like Benign Paroxysmal Positional Vertigo (BPPV) and Meniere’s disease arise from issues within these structures. In BPPV, tiny calcium crystals in the canals become dislodged, leading to brief episodes of intense spinning. Similarly, Meniere’s disease results from fluid build-up in the inner ear, resulting in fluctuating hearing loss and episodes of vertigo.
Understanding how the inner ear functions and the potential causes of its dysfunction can be vital for diagnosis and treatment. Through effective interventions, many individuals can manage or alleviate the debilitating symptoms associated with these disorders.
Impact of Neurological Conditions
Neurological disorders can profoundly affect the vestibular system and lead to disorders such as vestibular neuritis. This condition is caused by inflammation of the vestibular nerve, often due to viral infections. Individuals may experience severe vertigo that can last for days, severely affecting their quality of life. The acute onset of symptoms can be alarming and requires immediate medical attention for appropriate diagnosis.
Conditions like multiple sclerosis (MS) can also impact the vestibular pathways in the central nervous system. Patients with MS may experience episodes of vertigo due to demyelination in these pathways, which can disrupt the body’s balance signals. Such neurological impacts are important considerations when evaluating vestibular disorders.
Additionally, strokes may result in sudden balance problems and dizziness, indicating a more acute vestibular disorder. Immediate medical intervention is crucial in such cases as they may signify life-threatening events. Determining the underlying cause of vertigo due to neurological conditions is essential for effective treatment and management.
Understanding the relationship between neurological health and vestibular disorders can help in providing comprehensive care. Physical therapy and vestibular rehabilitation exercises can be effective in managing symptoms caused by these related conditions.
The Role of Environmental Factors
Environmental factors, such as head injuries and exposure to sudden changes in pressure, can significantly influence the development of vestibular disorders. Head trauma, even when seemingly minor, can disrupt the inner ear’s normal functioning, leading to dizziness and balance issues. Ensuring safety during activities that pose a risk of head injury is vital to prevent these kinds of disorders.
Another common environmental trigger is exposure to loud noises and pressure fluctuations, particularly when flying or diving. These conditions can lead to barotrauma, which affects the middle ear and can indirectly impact vestibular function. Individuals who frequently engage in activities involving pressure changes should be aware of the potential risk factors that could influence their vestibular health.
A less recognized factor is the role of stress and anxiety in exacerbating vestibular symptoms. Psychological stress can heighten awareness of dizziness and can even lead to conditions such as persistent postural-perceptual dizziness (PPPD). Individuals experiencing ongoing vestibular issues should consider their mental health and stress management practices as part of their overall treatment plan.
Addressing these environmental factors through preventive measures and awareness can substantially aid in reducing the incidence of vestibular disorders. A holistic approach to treatment should encompass both physical and psychological aspects to achieve the best possible outcomes for those affected.
Recognizing the Symptoms of Vestibular Disorders
Common Symptoms of Vestibular Disorders
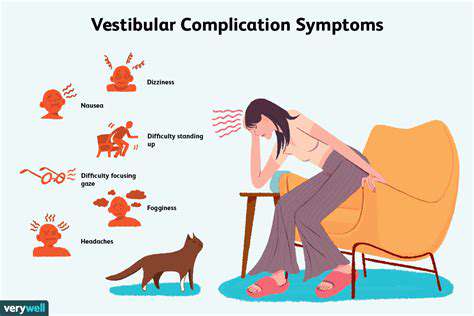
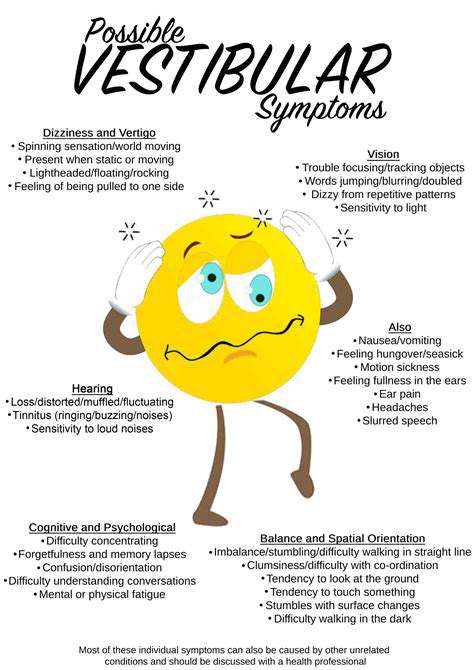
Vestibular disorders can produce a variety of symptoms that significantly impact daily life. Individuals often experience dizziness, which can range from a mild sensation of lightheadedness to a severe feeling of spinning known as vertigo. This dizziness is commonly accompanied by an unsteady gait that can lead to falls or injuries. Another prevalent symptom is imbalance, which may manifest during walking or standing still.
Tinnitus, or ringing in the ears, is another symptom frequently reported by those with vestibular issues. This auditory phenomenon can be distracting, making it difficult for individuals to concentrate and communicate effectively. Furthermore, hearing loss may also accompany vestibular disorders, affecting both the quality of life and the ability to engage in social activities.
In addition to dizziness and auditory symptoms, patients often report episodes of nausea. This nausea can be debilitating, causing reluctance to eat, which can lead to further complications. Understanding these symptoms is crucial for timely diagnosis and treatment of vestibular disorders. Equally concerning can be the psychological effects, as chronic dizziness and disorientation can lead to anxiety and depression.
Individuals may also experience visual disturbances. These disturbances may be characterized by difficulty focusing or seeing moving objects, a condition known as oscillopsia. Many patients struggle with their vision while in motion, which can hinder activities like driving or even walking through busy environments. Recognizing these symptoms early enhances opportunities for effective intervention and management.
The Impact of Vestibular Disorders on Daily Life
The symptoms of vestibular disorders can have profound effects on an individual's day-to-day functioning. Simple tasks such as walking or navigating stairs become increasingly challenging, which often leads to a decreased level of independence. For many, this loss of autonomy can significantly impact mental health and overall quality of life. Social interactions may diminish, as individuals often fear triggering episodes while engaging in common activities.
Workplace challenges also arise due to vestibular disorders. Many professions require stability and focus, and persistent dizziness can lead to absenteeism and reduced productivity. Patients might feel compelled to explain their symptoms to employers, which can lead to awkward conversations or misunderstandings. Hence, it’s essential for workplaces to foster awareness and understanding of such conditions.
Household responsibilities can also become overwhelming for those suffering from vestibular disorders. Activities that were once routine, such as cleaning or grocery shopping, may pose risks due to feeling unsteady. Families often need to find new ways to support loved ones coping with these challenges, further emphasizing the importance of raising awareness about vestibular disorders.
Additionally, the burden of these disorders is not only physical but also emotional. Individuals often experience feelings of frustration or isolation, especially if symptoms are difficult to communicate. Understanding this emotional landscape can help loved ones provide better support and encouragement. Building a strong support network is crucial for those navigating the complexities of vestibular disorders.
When to Seek Medical Attention for Vestibular Symptoms
Recognizing when to seek medical attention for vestibular symptoms is vital for effective diagnosis and treatment. If dizziness persists or worsens, particularly if accompanied by other concerning signs like severe headaches or blurred vision, it's critical to consult a healthcare provider. Prompt medical evaluation can help rule out serious underlying conditions that may mimic vestibular disorders. Additionally, individuals should look for sporadic episodes of vertigo or feelings of imbalance that disrupt their daily activities.
Another important indicator is the presence of hearing changes. If sudden hearing loss occurs alongside dizziness, immediate medical attention is needed. This combination can signify inner ear issues that require urgent care. Following up on these symptoms with a healthcare professional can lead to timely interventions, which can drastically improve outcomes.
Furthermore, if symptoms are triggered by specific movements or head positions—known as positional vertigo—a healthcare provider should be consulted. These symptoms may suggest benign paroxysmal positional vertigo (BPPV), which is usually treatable with targeted maneuvers. Understanding these triggers is essential for developing an effective management plan.
Lastly, it’s crucial to seek help when vestibular symptoms interfere with mental health. Feelings of anxiety, depression, or significant stress due to chronic dizziness should not be ignored, as they can compound the challenges of living with vestibular disorders. Engaging with a mental health professional can be beneficial, providing tools and strategies to cope with these emotional hurdles.
Diagnosis of Vestibular Disorders
Understanding the Diagnostic Process
Diagnosing vestibular disorders involves a thorough examination and various tests to pinpoint the root of the issue. The first step typically includes a detailed patient history where healthcare providers gather information about the patient's symptoms, frequency, and triggers. This information is crucial as it helps in tailoring the diagnostic approach. In some cases, patients may not immediately recognize their symptoms' significance, making this initial conversation vital.
After collecting the patient history, doctors generally perform a physical examination focusing on balance and coordination. Techniques such as observing eye movements and testing reflexes are standard practices. These examinations provide valuable insights into the vestibular system's functionality. Any abnormalities found during these tests can lead to further investigations or referrals to specialists.
Advanced diagnostic tools, such as MRI or CT scans, may also be utilized to rule out structural abnormalities or other neurological conditions. These imaging techniques play a key role in identifying problems that might not surface during physical tests. The results can reveal tumors, lesions, or vestibular nerve damage that could be contributing to the patient’s symptoms.
Vestibular testing is also a critical component of the diagnosis, with assessments such as electronystagmography (ENG) or videonystagmography (VNG) helping to evaluate inner ear function. These tests measure eye movements induced by head and body position changes, delivering insights into the vestibular system's functioning. The accuracy of these tests is vital for diagnosing specific types of vestibular disorders and determining appropriate treatment plans.
Common Diagnostic Tests for Vestibular Disorders
Many diagnostic tests are employed to analyze various aspects of the vestibular system's functionality. One of the most prominent tests is the caloric test, which checks how the inner ear responds to temperature changes. During this procedure, water or air at different temperatures is introduced into the ear canal, triggering eye movements that reflect vestibular activity. The results from this test can indicate whether the vestibular system is functioning correctly or if there is a dysfunction.
Another common test is the posturography test, which evaluates a person’s ability to maintain balance under different conditions. This test helps identify specific balance issues that may arise from vestibular disorders. Patients stand on a platform while their movements are monitored; responses to visual and tactile stimuli are also measured, providing insights into how well they can maintain stability.
The Head Impulse Test (HIT) is another critical examination in diagnosing vestibular disorders. In this test, the patient wears goggles that track eye movements while the head is quickly turned to one side. A normal response shows that the vestibular system is functioning well. In contrast, an abnormal response can suggest vestibular dysfunction, leading clinicians to make targeted recommendations for further evaluation or treatment.
Lastly, some specialists may opt for a thorough hearing test alongside vestibular evaluations since hearing and balance are closely linked. A comprehensive evaluation can help identify conditions such as Meniere's disease or vestibular migraines, which can manifest with both hearing loss and balance issues. This thorough assessment ensures a complete understanding of the disorder, paving the way for effective treatment options.
Treatment Options for Vestibular Disorders
Medications for Managing Vestibular Disorders
In the management of vestibular disorders, medications play a crucial role in alleviating symptoms such as dizziness, nausea, and imbalance. Commonly prescribed drugs include antihistamines like meclizine or dimenhydrinate, which help reduce motion sickness and vertigo. On the other hand, benzodiazepines can provide short-term relief of severe anxiety related to dizziness, but their use must be carefully monitored due to potential dependency issues.
Corticosteroids may be prescribed in cases of vestibular neuritis or labrynthitis to reduce inflammation and improve function. Other medications, such as prochlorperazine, may be utilized to address severe nausea associated with vestibular dysfunction. It’s essential for patients to discuss medication options thoroughly with their healthcare provider to tailor the treatment plan based on individual needs and potential side effects.
Moreover, ongoing research suggests that neuroprotective agents and vestibular rehabilitation exercises could enhance recovery outcomes when combined with pharmacologic treatments. This integrated approach helps optimize the management of vestibular disorders, providing patients with a more comprehensive and effective care strategy.
Physical Therapy and Vestibular Rehabilitation
Physical therapy, specifically vestibular rehabilitation therapy (VRT), is an essential treatment option for individuals suffering from vestibular disorders. VRT involves personalized exercises designed to improve balance, function, and reduction of dizziness through systematic exposure to movements that provoke symptoms. Over time, this approach helps the brain adapt and recalibrate to vestibular deficits.
Therapists typically utilize a variety of therapeutic maneuvers to address specific symptoms, such as the Epley maneuver for BPPV (Benign Paroxysmal Positional Vertigo), which facilitates the repositioning of displaced crystals within the inner ear. Tailored exercises, including gaze stabilization and balance training, are also incorporated into therapy sessions, providing a holistic approach to symptom alleviation.
Moreover, a strong patient-therapist relationship significantly impacts the success of vestibular rehabilitation therapy. Frequent assessments and adjustments to treatment plans ensure that individual progress is monitored and that any emerging issues are addressed promptly. By reinforcing coping strategies and fostering body awareness, VRT empowers patients to manage their conditions more effectively.
Surgical Interventions for Severe Cases
In some scenarios where vestibular disorders severely affect quality of life and unresponsive to conservative treatments, surgical options may be considered. Surgical interventions aim to correct anatomical issues or remove problematic structures within the vestibular system. For instance, labyrinthectomy or vestibular nerve section may be advised in cases of intractable Meniere's disease, specifically to alleviate vertigo.
Additionally, other surgical techniques such as intratympanic steroid injections have gained traction as minimally invasive outpatient procedures. These injections aim to reduce inflammation in the inner ear while preserving hearing function. Patient selection for surgery is critical, as potential risks and benefits must be carefully evaluated to ensure that the chosen method aligns with the overall health goals.
Post-surgical outcomes can vary widely, with some patients experiencing significant relief from symptoms, while others might not achieve their desired results. Continuous follow-up is essential to monitor recovery and implement further therapeutic measures if needed. Thus, a multidisciplinary approach involving otologists, neurologists, and physical therapists can enhance both surgical and non-surgical treatment effectiveness.