Understanding Chiari Malformation Type 1 (CM1)
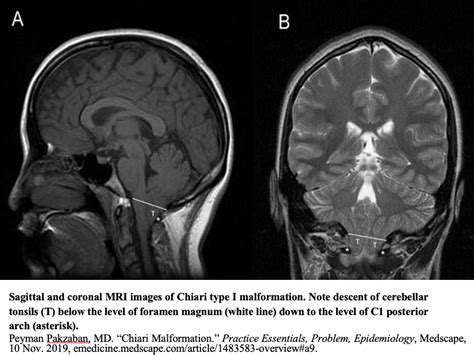
Chiari malformation type 1 (CM1) represents a neurological disorder where the cerebellum—the brain's coordination center—protrudes abnormally into the spinal canal. This anatomical variation creates a ripple effect throughout the nervous system. The resulting pressure on neural structures often manifests in ways that challenge both patients and clinicians to connect the dots between structure and symptoms.
While the cerebellum primarily governs motor control, its displacement in CM1 can disrupt cerebrospinal fluid flow and compress nearby nerves. This mechanical stress frequently translates into sensory disturbances and pain patterns that defy simple explanation. The complexity of these interactions underscores why CM1-related symptoms often evade immediate diagnosis.
The Mechanisms of Headache in CM1
Current research points to multiple overlapping processes that may generate headaches in CM1 patients. The mechanical theory suggests that cerebellar tonsils physically irritate pain-sensitive meningeal tissues during certain head movements. This mechanical irritation may explain why many patients report headache exacerbation during coughing, sneezing, or postural changes.
Simultaneously, emerging evidence highlights potential vascular components. The displaced cerebellum may compromise venous drainage from the brain, creating a form of intracranial hypertension. This vascular congestion could activate trigeminal nerve pathways—the same neural network implicated in migraine pathophysiology. Such dual mechanisms might account for the varied headache phenotypes observed clinically.
Headache Characteristics in CM1
CM1-related headaches typically demonstrate several distinguishing features. The pain often localizes to the occipital region with radiation toward the neck and shoulders, presenting as a persistent, pressure-like sensation. Unlike classic migraines, these headaches frequently intensify with Valsalva maneuvers—a clinical clue that often prompts neuroimaging.
Many patients describe a peculiar heavy head sensation that worsens as the day progresses. Some report accompanying symptoms like hand numbness or visual disturbances that fluctuate with headache intensity. This symptom constellation often serves as the first tangible evidence of underlying structural pathology.
Other Factors Contributing to Headaches
Secondary musculoskeletal changes frequently complicate the clinical picture. Chronic cerebellar dysfunction can lead to compensatory neck muscle overuse, creating tension-type headache components. Additionally, sleep disturbances—common in CM1 due to brainstem compression—may lower pain thresholds and perpetuate headache cycles.
The psychological impact of chronic pain shouldn't be underestimated. Many patients develop anxiety about symptom progression, which can amplify pain perception. This biopsychosocial complexity necessitates comprehensive evaluation beyond standard neurological exams.
Diagnosis and Management Strategies
Accurate diagnosis requires correlation between imaging findings and clinical symptoms. While MRI confirms cerebellar descent, the degree of herniation often poorly predicts symptom severity. Dynamic CSF flow studies sometimes reveal functional impairments not apparent on static images.
Treatment approaches must address multiple dimensions:
- Pharmacological options target specific symptoms (e.g., neuropathic pain medications)
- Physical therapy focuses on postural correction and cervical stabilization
- Surgical intervention remains reserved for cases with clear neurological progression
Identifying the Symptoms: Recognizing the Pattern
Understanding the Initial Signs
Symptom recognition poses particular challenges because CM1 manifestations evolve unpredictably. Early indicators might include subtle balance disturbances—perhaps occasional clumsiness or difficulty with tandem walking. Some patients report peculiar sensory phenomena, like transient tingling when turning their head.
These protean symptoms often lead to diagnostic odysseys spanning multiple specialists. The key to early identification lies in recognizing symptom patterns that defy conventional explanations—particularly when multiple neurological complaints coexist without clear cause.
Headaches and Associated Symptoms
The headache phenotype in CM1 often incorporates elements from multiple headache types. Patients may describe:
- Migraine-like photophobia combined with tension-type band-like pressure
- Exertional headache components resembling cardiac cephalalgia
- Positional elements suggestive of CSF leaks
Neurological Manifestations
Beyond headaches, CM1 can produce a spectrum of neurological oddities. Some patients develop unusual vocal changes—hoarseness or speech articulation difficulties—from vagus nerve involvement. Others experience temperature dysregulation or paradoxical sweating patterns suggesting autonomic dysfunction.
These manifestations reflect the brainstem's role as a neurological crossroads. When compressed, its diverse functions—from cranial nerve coordination to autonomic control—may become subtly impaired.
Cranial Nerve Dysfunction
Cranial nerve involvement often follows predictable patterns based on anatomical relationships. The trigeminal nerve (CN V) may cause facial pain mistaken for trigeminal neuralgia. Glossopharyngeal nerve (CN IX) irritation can produce throat pain or swallowing difficulties—sometimes prompting unnecessary ENT evaluations.
Vestibular Issues and Balance Problems
The vestibular symptoms in CM1 often present a diagnostic conundrum. Patients may describe:
- Positional vertigo resembling BPPV
- Constant disequilibrium like vestibular neuritis
- Exertional dizziness suggesting cardiovascular causes
Sensory Disturbances and Pain
The sensory abnormalities in CM1 often follow non-dermatomal patterns that confuse clinicians. Patients might report:
- Migratory tingling affecting different limbs at different times
- Thermal dysesthesia—burning sensations without apparent cause
- Proprioceptive distortions (e.g., feeling like limbs are positioned differently than they are)