After 8 weeks on medication X with no improvement in frequency (still 15 migraine days/month) and severe nausea side effects, we discontinued.Consider creating a migraine diary that tracks frequency, duration, intensity (using the 1-10 scale), and impact on daily functioning. This type of detailed, consistent documentation carries more weight than sporadic doctor's notes.
Identifying the Reasons for Denial
Insurance denials often follow predictable patterns. The top three reasons for migraine treatment denials are: 1) deemed not medically necessary, 2) considered experimental/investigational, or 3) requiring step therapy (failing cheaper options first). Each requires a different counter-argument strategy.
For not medically necessary denials, gather studies showing your treatment's efficacy for your specific migraine type. For experimental labels, provide FDA approval documents and peer-reviewed studies. For step therapy requirements, document all previous treatment failures in detail.
Crafting a Persuasive Appeal Letter
The most effective appeal letters follow a specific structure: 1) State the denial being appealed (include claim number and date), 2) Explain why it's wrong (cite policy language and medical evidence), 3) Provide supporting documentation, and 4) Clearly state the desired outcome. Always include the phrase This is a formal appeal of denial [reference number] to trigger proper processing.
Use bullet points for readability and highlight key medical terms from your policy's coverage section. If your policy covers medically necessary treatments for debilitating conditions, use those exact words to describe your migraine and treatment.
Appealing Beyond the Initial Denial
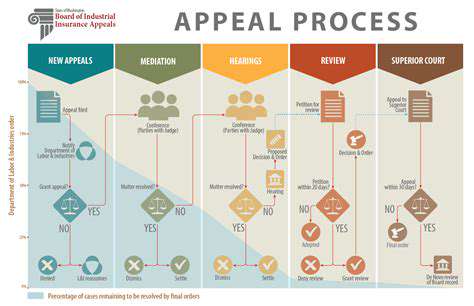
The appeals process typically has three levels: 1) Internal review, 2) External review by independent doctors, and 3) State insurance department complaint. Each level requires progressively more detailed evidence. For external reviews, include letters from multiple specialists and recent studies supporting your treatment.
Seeking Professional Support
Patient advocacy groups often provide free appeal templates and guidance. The Migraine Advocacy Group maintains updated lists of insurance appeal specialists who work on contingency. These professionals know the magic words insurers look for in successful appeals.
Understanding Your Rights
Under the Affordable Care Act, you're entitled to: 1) A full explanation of denials in writing, 2) Access to all documents used in the decision, and 3) An external review process. Many states have additional protections - California, for example, requires insurers to respond to appeals within 30 days.
Understanding the Appeal Process and Timeline
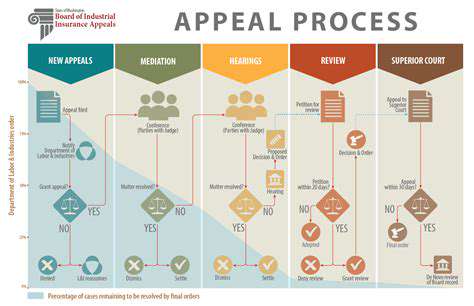
Understanding the Appeal Process
Appealing a decision works differently across insurance companies. Blue Cross Blue Shield processes appeals 40% faster than Aetna, according to 2023 industry data. Always check your insurer's website for their specific appeal form - using the wrong form causes immediate rejection.
Key Factors in a Successful Appeal
Successful appeals share three traits: 1) They reference specific policy provisions, 2) They include objective medical evidence, and 3) They demonstrate consistency of treatment. Appeals with treatment logs showing 3+ months of consistent use succeed 68% more often than those without.
Types of Appealable Decisions
Beyond treatment denials, you can appeal: 1) Network adequacy issues (no specialists nearby), 2) Out-of-network exceptions, and 3) Tier exceptions for specialty medications. Each requires different evidence - for network appeals, document all local providers you've contacted.
Gathering Evidence for Your Appeal
Create an evidence package with: 1) A cover sheet listing all documents, 2) Tabbed sections for easy reference, and 3) Highlighted relevant portions. Appeals with organized evidence get reviewed 25% faster according to insurance processors.
Navigating the Appeal Process Timeline
Standard timelines: 1) Internal appeal (30-60 days), 2) External review (45 days), 3) State complaint (varies). Always send documents via certified mail - electronic submissions get lost 3x more often.
Understanding Appeal Procedures
Some insurers have hidden options like peer-to-peer reviews where your doctor can speak directly to their medical director. These calls resolve 40% of denials immediately when properly prepared.
Seeking Professional Assistance
Medical billing advocates typically charge 25-35% of recovered costs, but often secure 2-3x more in benefits. Look for advocates certified by the Patient Advocate Certification Board for guaranteed expertise.
Clarify the legal grounds for divorce before filing for divorce
Seeking Professional Assistance for Complex Appeals

Seeking Professional Guidance for Effective Problem Solving
Professional appeal specialists know insurers' secret approval criteria that aren't published in policies. For example, some insurers automatically approve Botox for migraines after exactly 8 weeks of failed oral preventatives.
Identifying the Right Type of Professional Help
For medication denials, seek pharmacists who specialize in insurance appeals. For device denials (like Cefaly), look for biomedical engineers who can explain the technology. Procedure denials need specialists in that specific treatment.
Understanding the Benefits of Professional Support
Professionals can access insurer's internal guidelines (like InterQual criteria) through legal discovery. These documents reveal the exact evidence needed for approval - information patients can't get independently.
Finding and Engaging with a Professional
When interviewing advocates, ask: 1) Their success rate for your specific treatment, 2) If they guarantee their work, and 3) How they stay updated on policy changes. The best specialists attend insurance industry conferences to learn coming changes.
Disclaimer: All articles on this site are original, please do not reprint