Outline
Temporomandibular joint disorders can affect jaw movement and cause pain and headaches.
Jaw pain may trigger tension-type headaches due to muscle tension.
Bruxism is associated with jaw pain and headaches, often occurring during sleep.
Other issues, such as sinus infections, may also cause similar symptoms.
Preventive measures include stretching exercises and maintaining oral hygiene.
Professional therapies, such as physical therapy, can significantly relieve symptoms.
If symptoms persist or worsen, medical attention should be sought promptly.
Oral problems such as cavities and periodontal disease can lead to chewing pain.
Bruxism may exacerbate tooth sensitivity and headaches.
Preventive dental care can reduce the likelihood of pain occurrence.
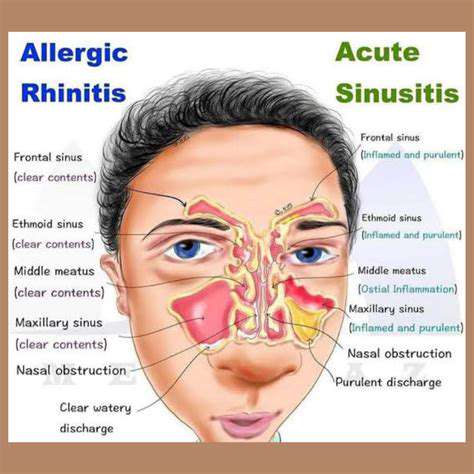
Radiating pain caused by sinusitis can affect the jaw and head.
Decongestants and home remedies are effective in treating sinusitis.
Nerve compression may lead to severe jaw and head pain.
Understanding neuropathic pain symptoms aids in early diagnosis.
Adjusting diet structure may help manage headaches during chewing.
Stress management techniques, such as mindfulness meditation, can alleviate discomfort during meals.
Consulting healthcare experts to create a personalized treatment plan is recommended.
Relationship Mechanism Between Jaw Pain and Headaches
Understanding Temporomandibular Joint Disorders (TMJ)
Temporomandibular joint disorders are a series of conditions affecting the jaw joint and surrounding muscles. Statistics show that approximately 10 million people in the U.S. are troubled by this, with common symptoms including limited jaw movement and headaches. The manifestation of the condition varies significantly, with mild cases only feeling discomfort and severe cases experiencing persistent pain.
The causes are complex and varied, possibly involving jaw injuries, arthritis, or nighttime bruxism. Notably, mental stress is also a significant trigger—when a person is anxious, they often unconsciously clench their teeth, exacerbating the symptoms.
During diagnosis, doctors combine palpation and imaging assessments. X-rays or MRIs can clearly observe the joint structure, and sometimes occlusal analysis is needed to determine the treatment plan.
The Mechanism of Jaw Pain Triggering Headaches
Referred pain generated from the tension in the jaw muscles can radiate to the temporal region, forming tension-type headaches. Research published in the Journal of Craniofacial Surgery shows that 70% of patients with jaw pain also have headache symptoms. This association is closely related to the conduction pathway of the trigeminal nerve—when this nerve is stimulated, pain signals are transmitted to both the jaw and head simultaneously.
Unusual occlusal forces generated by nighttime bruxism can reach up to 6 times normal chewing pressure; this continuous load not only damages teeth but can also lead to throbbing pain at the temples upon waking. Clinical findings indicate that the use of customized occlusal splints can reduce headache frequency in 80% of patients.
The Hidden Pain Instigator: Bruxism
About 20% of adults experience sleep bruxism, an unconscious behavior that can lead to excessive fatigue of the chewing muscles. Long-term bruxism not only wears down tooth enamel but can also alter occlusal relationships, creating a vicious cycle. In addition to customized dental splints, cognitive-behavioral therapy has been shown to effectively relieve stress-induced bruxism.
Those experiencing the following symptoms should seek medical attention promptly: jaw stiffness upon waking, abnormal tooth wear, and tenderness in the preauricular area. Timely intervention can prevent secondary headaches from becoming chronic.
Other Causes That Shouldn't Be Ignored
The maxillary sinus is anatomically adjacent to the oral cavity; when sinusitis occurs, pressure from purulent secretions can stimulate the superior alveolar nerve, creating a toothache-like illusion. This condition is often accompanied by facial swelling and orthostatic headaches, and using sinus rinses combined with antibiotics can provide rapid relief.
Furthermore, poor posture with forward-leaning necks can cause continuous tension in the sternocleidomastoid muscle; this tension can be transmitted through the fascial chain to the chewing muscles. It is advisable for desk workers to perform neck stretches every 45 minutes and to use ergonomic office equipment.
The Impact of Oral Issues on Pain
Common Oral Diseases That Cause Pain
Severe tooth decay that exposes the pulp can directly stimulate the dental nerve during chewing, causing sharp pain. The World Health Organization reports that 35% of chewing pain arises from untreated cavities. The initial symptoms of tooth fractures are subtle, but a brief sharp pain when biting on hard objects is an important warning sign.
Late-stage periodontitis can result in loose teeth, making chewing feel like stepping on loose stones, not only causing pain but also potentially accelerating tooth loss. Regular dental cleanings can remove 90% of pathogenic plaque, making it an effective means of preventing periodontal disease.
The Invisible Destroyer: Nocturnal Bruxism
Sleep monitoring shows that bruxers experience periodic muscle electrical bursts during REM sleep. This abnormal activity causes soreness in the chewing muscles upon waking, akin to having just run a marathon, accompanied by radiating temporal headaches. Biofeedback therapy can remind individuals to interrupt the bruxing action through vibration, and combined with relaxation training, the results can be more effective.
Response Strategies and Lifestyle Adjustments
Dietary Improvement Plan
Replacing steak with fish balls and nuts with steamed pumpkin can reduce chewing load by 60%. Patients with swallowing difficulties might try spoon-fed meals—processing food into a pudding-like consistency ensures nutritional intake while avoiding excessive effort.
Stress Management System
Progressive muscle relaxation techniques can effectively relieve jaw tension: inhale while tightening the chewing muscles for 5 seconds, then fully relax while exhaling, repeating for 10 sets. Those in the office can set phone reminders to perform 1-minute 'smile exercises' every hour—lifting the corners of the mouth until a mild strain is felt can help naturally relax tense muscles.
Timing for Professional Intervention
Seek medical attention immediately when the following conditions arise: mouth opening less than two fingers wide, pain affecting sleep, accompanied by tinnitus or dizziness. The latest treatment guidelines recommend a multidisciplinary collaborative treatment model, with cooperation between dental and physiotherapy departments to develop rehabilitation plans.