Hiểu về Mối Kết Nối
Đau đầu mãn tính thường xuyên
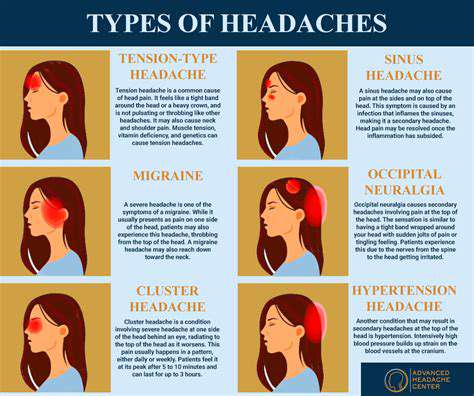
Các loại đau đầu thường gặp ở bệnh nhân hội chứng tăng nhạy cảm (EDS)
Read more about Hội chứng Ehlers-Danlos (EDS) và tỷ lệ mắc đau đầu tăng lên
Chiến Lược Hiệu Quả Để Quản Lý Cơn Đau Cổ Kinh Niên
Giải Pháp Hiệu Quả Để Giảm Đau Cổ. Khám phá các nguyên nhân phổ biến gây ra cơn đau cổ, bao gồm căng cơ, chấn thương, bệnh thoái hóa đĩa đệm và căng thẳng. Hướng dẫn toàn diện này khám phá các kỹ thuật quản lý cơn đau thực tiễn như bài tập vật lý trị liệu, điều chỉnh công thái học và các phương pháp chánh niệm. Tìm hiểu tầm quan trọng của việc tham khảo ý kiến các chuyên gia y tế để có các kế hoạch điều trị cá nhân hóa và cách duy trì lối sống lành mạnh có thể ngăn ngừa tái phát. Tìm sự giảm nhẹ cơn đau cổ kinh niên và cải thiện sức khỏe tổng thể của bạn ngay hôm nay.
Chiến Lược Hiệu Quả Để Quản Lý Đau Xoang Ở Đằng Sau Đầu
Nguyên nhân, Triệu chứng và Chiến lược Giảm nhẹ. Tìm hiểu về các nguyên nhân khác nhau gây đau xoang ở đằng sau đầu và cách hiểu về giải phẫu xoang đóng vai trò quan trọng trong việc xác định các yếu tố kích thích và triệu chứng. Các yếu tố phổ biến như dị ứng, nhiễm trùng xoang và chất kích thích từ môi trường có thể dẫn đến sự khó chịu đáng kể ảnh hưởng đến cuộc sống hàng ngày. Khám phá các biện pháp tự chăm sóc hiệu quả, bao gồm bổ sung nước, hít hơi nước và các loại thuốc không kê đơn có thể giảm triệu chứng. Hướng dẫn của chúng tôi cũng nhấn mạnh tầm quan trọng của việc nhận biết khi nào cần tìm kiếm sự giúp đỡ chuyên nghiệp, đảm bảo can thiệp kịp thời cho các triệu chứng kéo dài hoặc nghiêm trọng. Khám phá các biện pháp điều trị tại nhà đã được kiểm chứng cùng với những thay đổi trong lối sống có thể cải thiện sức khỏe xoang và giảm tần suất đau. Giữ thông tin về tình trạng của bạn và tự trang bị cho mình các chiến lược để quản lý hiệu quả và giảm nhẹ cơn đau xoang ở đằng sau đầu.
Đau đớn: Chất xúc tác ẩn giấu cho sự phát triển và khả năng phục hồi
đau, phát triển bản thân, khả năng phục hồi, vượt qua thử thách, đồng cảm, lòng tự thương, chuyển hóa, hỗ trợ cộng đồng
Khám Phá Những Phức Tạp Của Nỗi Đau Ở Cấp Độ Cơ Bản
Mô tả Trang Web cho "Bản Chất của Nỗi Đau và Tác Động của Nó đến Cuộc Sống" Khám phá bản chất đa diện của nỗi đau và những tác động sâu sắc của nó đến cuộc sống của cá nhân trong bài viết toàn diện của chúng tôi. Tìm hiểu về các khía cạnh sinh học và tâm lý của nỗi đau, bao gồm nỗi đau cảm giác và nỗi đau thần kinh, cũng như vai trò quan trọng của sự hỗ trợ xã hội và các yếu tố kinh tế xã hội trong việc nhận thức và quản lý nỗi đau. Phân tích của chúng tôi đào sâu vào các tác động của nỗi đau mãn tính, các chiến lược giảm đau đổi mới và những tiến bộ công nghệ mới nhất trong quản lý đau. Bằng cách hiểu sự tương tác giữa sức khỏe cảm xúc và sự khó chịu về thể chất, tìm ra các phương pháp toàn diện hiệu quả, chiến lược đối phó và tầm quan trọng của các quan điểm văn hóa trong điều trị đau. Nhận thông tin về các liệu pháp tích hợp và cách chúng có thể giúp cá nhân quản lý nỗi đau của họ một cách hiệu quả trong khi nâng cao chất lượng cuộc sống.
Đau âm ỉ ở gáy: Nguyên nhân phổ biến và giải pháp
Khám phá các nguyên nhân phổ biến gây ra đau âm ỉ ở gáy, từ căng cơ và strain đến chứng đau nửa đầu và các vấn đề về cột sống cổ. Hướng dẫn thông tin này đề cập đến các triệu chứng cần lưu ý, khi nào nên tìm kiếm sự chăm sóc y tế và các lựa chọn điều trị hiệu quả, bao gồm thuốc không kê đơn, liệu pháp nhiệt và các kỹ thuật quản lý căng thẳng. Tìm hiểu cách các yếu tố lối sống có thể ảnh hưởng đến tần suất đau đầu và khám phá các biện pháp phòng ngừa để giảm khó chịu và cải thiện sức khỏe tổng thể. Hãy giữ cho mình thông tin về sức khỏe và áp dụng các chiến lược chủ động để kiểm soát cơn đau.
Ô nhiễm tiếng ồn: Một tác nhân gây đau đầu môi trường bị bỏ qua
Ô nhiễm tiếng ồn: Một tác nhân gây đau đầu môi trường bị bỏ qua
Xây dựng lối sống phòng ngừa cho chứng đau đầu dữ dội mãn tính
Xây dựng lối sống phòng ngừa cho chứng đau đầu dữ dội mãn tính
Hiểu về Hội chứng Đau đầu Migraine kéo dài: Khi cơn đau đầu không ngừng
Hiểu về Hội chứng Đau đầu Migraine kéo dài: Khi cơn đau đầu không ngừng
Suy giảm chức năng ty thể và mối liên hệ tiềm năng với năng lượng đau nửa đầu
Suy giảm chức năng ty thể và mối liên hệ tiềm năng với năng lượng đau nửa đầu
Chống chỉ của thuốc Triptan: Ai nên tránh sử dụng?
Chống chỉ của thuốc Triptan: Ai nên tránh sử dụng?
Đạo đức của việc sử dụng giả dược trong các thử nghiệm lâm sàng về chứng đau nửa đầu
Đạo đức của việc sử dụng giả dược trong các thử nghiệm lâm sàng về chứng đau nửa đầu
Đề cập đến định kiến về sức khỏe tâm thần trong cộng đồng người bị đau nửa đầu
Đề cập đến định kiến về sức khỏe tâm thần trong cộng đồng người bị đau nửa đầu