The Prevalence of Migraines in Students
The Impact of Stress on Migraine Frequency
Academic pressures, social anxieties, and extracurricular demands create a perfect storm for student stress. When stress becomes chronic, the body often responds with more frequent and intense migraines, revealing the undeniable connection between mental strain and physical symptoms. While counseling and stress management won't eliminate migraines completely, they can significantly reduce their frequency and severity.
The modern student faces unprecedented pressure - from maintaining perfect grades to building impressive resumes while navigating complex social dynamics. This constant performance anxiety creates physiological changes that trigger migraines in susceptible individuals. Recognizing these pressure points allows for targeted interventions that can break the stress-migraine cycle.
The Role of Sleep Deprivation
Sleep deprivation has become a badge of honor among overachieving students, yet it's one of the most potent migraine triggers. The brain's pain modulation systems become dysregulated without proper rest, lowering the threshold for migraine attacks. Simple changes like establishing a consistent bedtime routine and limiting screen time before sleep can yield dramatic improvements.
Dietary Factors and Migraine Triggers
Students often overlook how their eating habits influence migraine patterns. Skipping meals, excessive caffeine consumption, and reliance on processed snacks create blood sugar fluctuations that can trigger headaches. Keeping a food diary helps identify personal triggers, allowing students to make informed dietary choices without unnecessary restrictions.
Genetic Predisposition and Family History
If migraines run in the family, students should view this as valuable predictive information rather than inevitable fate. Understanding one's genetic vulnerability enables proactive management rather than reactive treatment. This knowledge empowers students to implement preventive strategies before migraines significantly impact their academic performance.
Environmental Factors and Migraine Induction
Classroom fluorescent lighting, strong laboratory chemicals, and even sudden weather changes can serve as unexpected migraine triggers. Simple adaptations like wearing sunglasses outdoors or requesting seating away from bright lights can make classrooms more migraine-friendly environments.
The Importance of Early Diagnosis and Intervention
Migraines left undiagnosed often lead to unnecessary academic struggles. Early identification allows for classroom accommodations like extended test times or permission to wear sunglasses indoors. School nurses trained to recognize migraine symptoms can be invaluable allies in getting students appropriate care.
The Significance of Managing Chronic Pain
For students with frequent migraines, developing a comprehensive pain management plan is as crucial as any academic strategy. This might include scheduled medication, biofeedback training, or even cognitive behavioral therapy. When schools, families, and healthcare providers collaborate, students learn to manage their condition rather than being controlled by it.
Identifying and Assessing Migraine Symptoms in Students
Understanding Migraine Triggers
Migraines represent more than just severe headaches - they're complex neurological events with distinct phases. Identifying personal triggers requires detective-like observation, noting not just obvious factors but subtle patterns in sleep, hydration, and activity levels preceding attacks.
While common triggers like stress and certain foods affect many, each student's migraine profile is as unique as their fingerprint. Some may react to hormonal changes, others to specific weather patterns or sensory stimuli. This individualized nature makes trigger identification both challenging and essential.
Assessing Migraine Severity and Frequency
Effective migraine management begins with accurate tracking. A detailed headache diary should record not just pain levels, but associated symptoms like nausea, visual disturbances, and cognitive changes. This data reveals patterns that simple pain descriptions might miss.
Frequency tracking proves particularly valuable - students often don't realize how often migraines disrupt their lives until they see the numbers. This objective evidence helps justify medical interventions or academic accommodations when needed.
Diagnostic Criteria and Evaluation
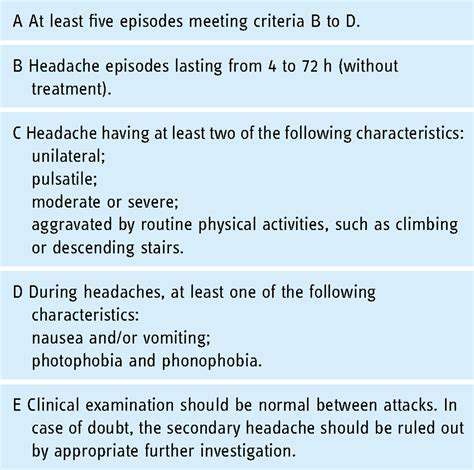
Proper migraine diagnosis requires more than just describing head pain. Neurologists look for specific symptom clusters including unilateral throbbing, light/sound sensitivity, and nausea lasting 4-72 hours. Students should prepare detailed descriptions of their experiences before medical appointments.
The International Headache Society criteria provide a standardized framework, but atypical presentations are common in younger patients. Abdominal migraines or aura without headache can be particularly confusing without professional evaluation.
Managing Migraine Pain and Symptoms
Effective migraine management requires a multi-pronged approach. Acute treatments work best when taken at the first warning signs, while preventive strategies aim to reduce attack frequency. Non-pharmacological approaches like cold therapy or quiet dark rooms complement medication for many students.
The most successful treatment plans evolve over time as students learn what works for their unique migraine patterns. Regular follow-ups ensure adjustments keep pace with changing symptoms and lifestyle factors.
Developing Personalized Management Strategies

Understanding the Core Principles of Personalized Management
Personalized migraine management begins with recognizing that no two students experience migraines identically. Effective strategies must account for academic schedules, extracurricular commitments, and personal coping styles. This tailored approach yields better adherence and outcomes than generic advice.
Open communication between students, parents, and healthcare providers forms the foundation. Students often withhold information about migraine impacts fearing academic consequences. Creating a safe space for honest discussion leads to more effective solutions.
Tailoring Strategies for Optimal Performance
Academic accommodations should address the student's specific migraine patterns. A student with morning migraines might benefit from later start times, while one sensitive to fluorescent lights may need permission to wear tinted glasses. These targeted adjustments minimize disruptions while maintaining academic standards.
Identifying and Addressing Individual Needs
Beyond medical treatment, students often need help navigating migraine's social and emotional impacts. Fear of public attacks or being labeled fragile creates significant anxiety. Support groups or counseling can help students develop coping strategies and self-advocacy skills.
Implementing Personalized Performance Reviews
Regular check-ins help assess whether management strategies remain effective as students grow and circumstances change. What worked freshman year may need adjustment by junior year as academic pressures increase. These reviews should consider both headache metrics and overall wellbeing.
Measuring and Evaluating the Effectiveness of Personalized Management
Success shouldn't be measured solely by migraine frequency. Improved school attendance, better stress management, and maintained social connections are equally important outcomes. Tracking these broader metrics provides a more complete picture of intervention effectiveness.
Implementing Preventive and Proactive Measures
Early Detection and Intervention
School health professionals serve as frontline detectors of emerging migraine patterns. Training teachers to recognize subtle signs like squinting or withdrawal during pre-headache phases can facilitate early intervention. Simple measures like allowing a break at prodrome signs might prevent full attacks.
Promoting Healthy Lifestyles
Wellness programs should address migraine-specific needs beyond general health advice. Hydration stations, stress-reduction spaces, and migraine-friendly lighting options create supportive environments. Educating the entire school community reduces stigma and fosters understanding.
Developing Crisis Response Plans
Clear migraine protocols prevent unnecessary emergency room visits while ensuring student safety. Designated quiet recovery spaces with dim lighting allow students to manage attacks with dignity. Staff training ensures consistent, appropriate responses across all school settings.
Collaboration and Communication
Effective migraine management requires breaking down silos between medical, academic, and administrative staff. Shared digital platforms can coordinate accommodations while maintaining student privacy. Regular team meetings ensure all stakeholders remain informed and aligned.
Injury Prevention and Safety Measures
For students with migraine-related dizziness or visual disturbances, simple classroom modifications improve safety. Non-slip flooring, clearly marked steps, and obstacle-free pathways reduce fall risks during aura phases. These universal design principles benefit all students while specifically supporting those with migraines.