What is Occipital Bone Pain?
Understanding Occipital Bone Pain
Occipital bone pain refers to discomfort or pain that originates from the occipital bone, located at the back of the skull. This type of pain can range from mild to severe and can be a result of various underlying conditions. It’s important to understand the anatomy of the occipital region to grasp why pain may occur in this area.
The occipital bone is responsible for protecting the brain and providing structural support for the head. Pain in this area can often be linked to tension or strain in nearby muscles, as well as nerve irritation. These factors can lead to a variety of painful sensations, including sharp, aching, or throbbing pain.
Individuals experiencing occipital bone pain may also report accompanying symptoms such as headaches, neck stiffness, or discomfort that radiates towards the eyes or ears. Identifying the specific nature of the pain is essential for effective diagnosis and treatment.
In some cases, occipital pain may be chronic, leading to ongoing discomfort that significantly impacts daily activities. Understanding the causes of such pain is crucial for developing a tailored approach to treatment.
Ultimately, recognizing occipital bone pain and its potential causes can help individuals seek appropriate medical advice and pursue effective treatments to improve their quality of life.
Common Causes of Occipital Bone Pain
Several factors can contribute to occipital bone pain. One of the most prevalent causes is tension-type headaches, which are often a result of stress, poor posture, or muscle tension in the neck and upper back. Such headaches can generate significant discomfort at the base of the skull.
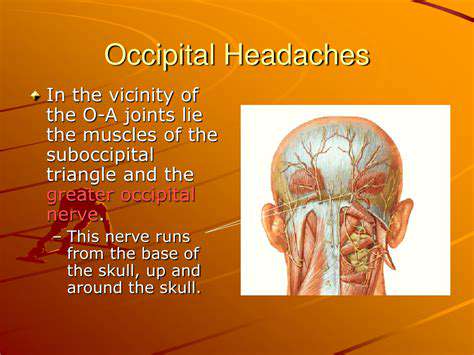
Another common cause is occipital neuralgia, a condition resulting from irritation or injury to the occipital nerves. This irritation can lead to sharp, shooting pain that often mimics headaches and may be exacerbated by movements of the neck.
Injuries, such as whiplash from car accidents or falls, can also result in occipital bone pain. These injuries can strain the surrounding muscles and ligaments, leading to inflammation and discomfort in the occipital area.
Furthermore, certain medical conditions, including arthritis, can contribute to pain in the occipital region. Inflammation of the joints in the cervical spine can cause referred pain that extends to the occipital bone.
Lastly, lifestyle factors such as lack of physical activity, improper ergonomics at work, and prolonged screen time can lead to muscle fatigue and tension that fuels occipital pain. Awareness of these factors can aid in prevention and management.
Diagnosis of Occipital Bone Pain
To accurately diagnose the cause of occipital bone pain, healthcare professionals typically begin with a thorough patient history and physical examination. This process helps to identify the characteristics of the pain, its duration, and any associated symptoms.
Healthcare providers may also utilize imaging studies, such as X-rays, MRI, or CT scans, to look for structural abnormalities or signs of injury in the cervical spine and surrounding areas. These tests can provide insight into whether a more serious condition is contributing to the pain.
Additionally, neurological evaluations are often performed to assess the function of the occipital nerves and determine if neuralgia is present. These evaluations can help differentiate between various types of headaches and pain syndromes.
Patients are encouraged to keep a pain diary, noting when the pain occurs, its intensity, and any activities or triggers that may exacerbate it. This information can be invaluable for healthcare providers in making an accurate diagnosis.
Early and accurate diagnosis is key to effective treatment, allowing for targeted interventions that can alleviate pain and improve patient outcomes.
Treatment Options for Occipital Bone Pain
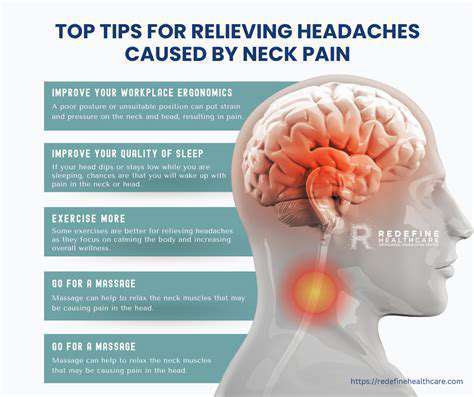
Treatment for occipital bone pain largely depends on the underlying cause. For tension-related pain, lifestyle modifications such as stress management techniques, regular exercise, and improved ergonomics can be beneficial. Gentle neck stretches and relaxation exercises may also help relieve muscular tension.
In cases of occipital neuralgia, healthcare providers may recommend medications such as anti-inflammatories, muscle relaxants, or nerve block injections to alleviate pain. Physical therapy can also play a crucial role in rehabilitation and pain management.
For individuals suffering from chronic pain, alternative therapies such as acupuncture, chiropractic adjustments, and massage therapy may provide relief by addressing muscle tension and enhancing overall well-being.
In more severe instances, surgical options may be considered for decompression of the occipital nerves or addressing structural issues that contribute to pain. However, these options are typically reserved for cases that do not respond to conservative treatments.
Ultimately, a multidisciplinary approach involving healthcare professionals, physical therapists, and pain specialists can provide comprehensive care and support for individuals coping with occipital bone pain.
Common Causes of Occipital Bone Pain
Muscle Tension and Strain
One of the most common causes of occipital bone pain is muscle tension and strain. This can occur due to poor posture, prolonged sitting, or repetitive movements. Over time, these factors can lead to tightness in the muscles surrounding the occipital region.
Individuals with muscle tension often describe the pain as a dull ache or a throbbing sensation. To alleviate this discomfort, regular stretching and strengthening exercises can be beneficial.
Injuries and Trauma
Injuries to the head or neck can also result in pain around the occipital bone. Trauma from accidents, falls, or sports can lead to inflammation and soreness in this area. It's essential to seek medical advice if the pain persists following an injury.
In addition to immediate treatment, rehabilitation techniques may be necessary to restore proper function. Physical therapy can play a critical role in recovery and pain management.
Medical Conditions
Certain medical conditions can contribute to the occurrence of occipital bone pain. For instance, ailments like migraines and cervical spondylosis can cause pain that radiates to the occipital area. Understanding these underlying conditions is crucial for effective treatment.
Management of these conditions may involve medication, lifestyle changes, or alternative therapies. Patients should consult healthcare professionals for tailored approaches to their specific conditions.
Treatment Options
There are various treatment options available for managing occipital bone pain. Common approaches include physical therapy, medication, and lifestyle modifications to reduce strain on the neck and upper back. In some cases, interventions such as nerve blocks may be considered.
Holistic treatments, such as acupuncture and massage therapy, can also provide relief. Patients are encouraged to explore different options in consultation with healthcare providers to find the most effective and suitable treatment.
When to Seek Medical Attention
Understanding the Signs of Serious Conditions
While occipital bone pain can often be attributed to muscle tension or poor posture, certain symptoms may indicate a more severe underlying condition. These can include severe headaches, visual disturbances, or neck stiffness. Recognizing these signs early on is crucial for effective intervention.
In cases where pain is accompanied by neurological symptoms, such as weakness or numbness in the limbs, it is vital to seek immediate medical attention. These symptoms could suggest that the pain is connected to issues affecting the nervous system, which require prompt evaluation.
It is also essential to monitor the duration and intensity of the pain. If the discomfort worsens or does not improve with typical home care methods, it may necessitate a visit to a healthcare professional for further assessment.
Evaluating Personal Health History
Your personal health history plays a significant role in determining whether to seek medical help for occipital bone pain. Conditions such as migraines, recent injuries, or chronic ailments can exacerbate headaches or pain in this region.
A detailed account of previous medical conditions, surgeries, and even medication use can provide valuable information to your healthcare provider. This context will assist them in diagnosing the source of the pain and determining the most suitable treatment plan.
Additionally, if there is a family history of neurological or chronic conditions, it may increase the impetus to consult a healthcare professional sooner rather than later, as it can reveal genetic predispositions to certain health issues.
When Home Remedies Are Not Enough
Many individuals attempt to manage occipital bone pain with home remedies such as rest, ice, heat therapy, or over-the-counter pain relief medications. However, there are times when these strategies may not be sufficient to alleviate the pain.
If you find that your symptoms persist despite trying various home treatments, it's a clear indication that professional medical evaluation is necessary. Inadequate response to initial care may suggest that the underlying cause is more complex and requires targeted treatment interventions.
Moreover, if home remedies lead to adverse effects or increased discomfort, this signals a need for professional guidance. A healthcare provider can offer tailored solutions, including physical therapy, stronger medications, or other therapeutic options to address the persistent pain effectively.
Treatment Options for Occipital Bone Pain
Understanding Occipital Bone Pain
Occipital bone pain, also known as occipital neuralgia, is a type of headache that originates from irritation or injury to the occipital nerves. These nerves, located at the back of the head, can become inflamed, leading to intense pain that radiates down the neck. Understanding the nuances of this condition is essential for effective management and treatment.
The pain associated with occipital bone issues can manifest as sharp, throbbing, or aching sensations. Patients often describe the discomfort as similar to a migraine but localized at the base of the skull. Identifying the specific symptoms and their onset can be crucial for proper diagnosis.
Common causes include muscle tension, pinched nerves, and underlying conditions such as arthritis or trauma to the neck. Recognizing these triggers plays a significant role in developing a comprehensive treatment plan.
Doctors typically rely on patient history, physical examinations, and imaging studies to diagnose the condition accurately. Awareness of the signs and symptoms can help individuals seek timely medical attention and avoid chronic pain.
Conservative Treatment Approaches
For many patients suffering from occipital bone pain, conservative treatment options can offer significant relief. These methods are often tried before moving on to more invasive procedures. They typically include physical therapy and manual manipulation to relieve tension in the neck and upper back.
Another common approach involves the use of heat or ice therapy. Applying heat can help relax tight muscles, while ice can reduce inflammation in the affected areas. Both methods can easily be incorporated into a patient’s daily routine.
Additionally, over-the-counter pain medications such as ibuprofen or acetaminophen can be effective in managing pain and discomfort associated with occipital neuralgia. However, it’s crucial for patients to consult healthcare providers to determine the best course of action, especially if pain persists.
Stress management techniques, such as yoga and meditation, may also play a role in minimizing the frequency and intensity of pain episodes. A holistic approach to treatment can enhance overall well-being and reduce the likelihood of recurrent issues.
Advanced Treatment Options
In cases where conservative treatments fail to alleviate pain, doctors may recommend more advanced options. Nerve blocks, where anesthetic agents are injected around the occipital nerves, can provide essential relief for some individuals. This procedure not only diminishes pain but also aids in establishing a clearer diagnosis.
In more chronic or severe cases, patients may benefit from neuromodulation therapies. These less invasive procedures involve the implantation of devices that send electrical impulses to the occipital nerves, interrupting pain signals before they reach the brain.
Surgery may be considered as a last resort, particularly if there is a structural issue contributing to nerve irritation. Surgical options vary depending on the underlying cause and can range from decompression techniques to more extensive surgical interventions.
Integrating multiple treatment modalities can be essential for optimal patient outcomes, and ongoing communication with healthcare providers is crucial to tailor the treatment plan as symptoms evolve. Patients are encouraged to discuss all options thoroughly to make informed decisions about their care.
Preventing Occipital Bone Pain
Understanding the Risk Factors
Occipital bone pain can be induced by various risk factors, which are essential to identify for effective prevention. Common contributors include poor posture, prolonged screen time, and lack of ergonomic support.
Additionally, individuals with previous neck injuries or tension headaches may find themselves more susceptible. Recognizing these risk factors early can significantly reduce the likelihood of experiencing pain in the occipital region.
Effective Lifestyle Adjustments
Making simple lifestyle adjustments can play a crucial role in preventing occipital bone pain. Incorporating regular breaks from screen time, practicing good posture, and ensuring proper ergonomic setups can greatly alleviate strain on the neck.
Furthermore, engaging in neck-strengthening exercises and stretching routines can provide added resilience against potential discomfort. These proactive measures create a supportive environment for overall neck health.
The Role of Professional Guidance
Seeking professional guidance is pivotal in managing and preventing occipital bone pain effectively. Consultation with physical therapists or chiropractors can yield tailored exercises and treatments aligned with individual needs. These specialists can also help educate patients on the importance of body mechanics and ergonomics.
Moreover, regular check-ups can aid in early detection of any underlying issues that may contribute to pain. Establishing a relationship with health professionals equips individuals with the tools to mitigate pain and enhance their quality of life.