A Key Player in Migraine PathophysiologyCalcitonin gene-related peptide (CGRP) is a prominent neuropeptide implicated in the development of migraine. Its presence in high concentrations in the cerebrospinal fluid and at migraine pain sites suggests a significant role in the inflammatory response and vasodilation contributing to migraine attacks. Research into targeting CGRP has yielded promising results, demonstrating its importance as a potential therapeutic target.
Substance P: Sensitizing the Nervous System
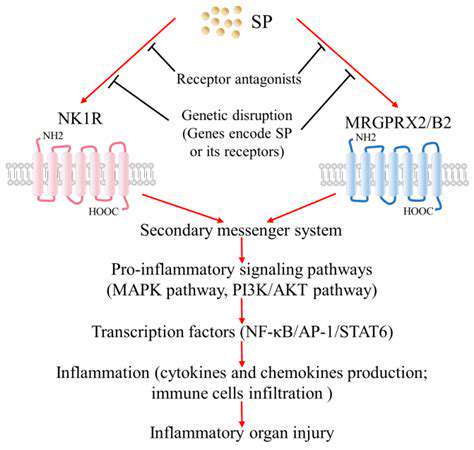
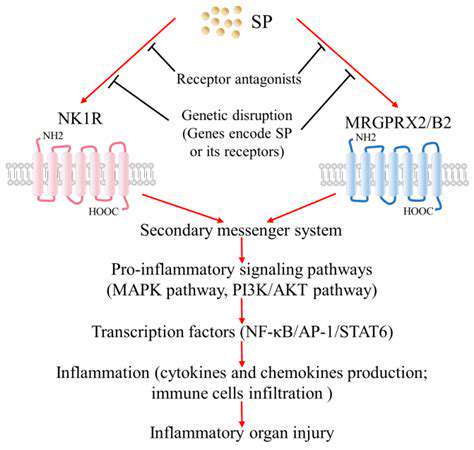
Substance P, another crucial neuropeptide, is linked to the sensitization of pain pathways. Its involvement in nociception, the process of perceiving pain, suggests a key role in the amplification of pain signals during a migraine attack. Understanding how substance P interacts with other neuropeptides and neurotransmitters is essential to unravel the complex mechanisms underlying migraine.
VIP and SP: Exploring Further Neuropeptide Involvement
Vasopressin-related peptides (VIP) and somatostatin (SP) also play a part in the intricate peptide landscape of migraine. VIP, for example, is known to have vasodilatory properties, potentially contributing to the vascular changes observed during a migraine attack. Somatostatin, on the other hand, exhibits a range of effects, including modulating inflammation and neurotransmission, suggesting a broader influence on migraine pathophysiology.
The Interplay of Neuropeptides and Other Signaling Pathways
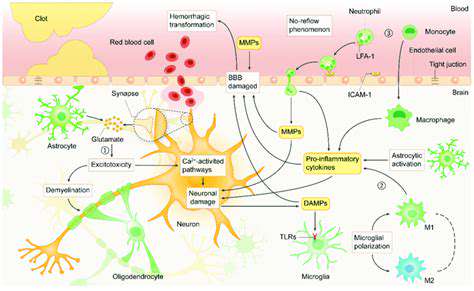
The involvement of neuropeptides in migraine isn't isolated; it's intertwined with other signaling pathways. The interactions between neuropeptides and neurotransmitters, such as serotonin and glutamate, likely contribute to the complex cascade of events that initiate and perpetuate a migraine attack. Investigating these interactions holds the potential to unveil novel therapeutic avenues.
Future Directions in Neuropeptide Research for Migraine Treatment
Targeting specific neuropeptides or their receptors presents exciting possibilities for developing innovative migraine treatments. Future research should focus on identifying novel neuropeptide targets and exploring the use of selective antagonists or agonists to modulate their activity. Developing a deeper understanding of the intricate network of neuropeptides and their interactions with other signaling pathways could revolutionize our approach to migraine management.
Beyond CGRP: Exploring Other Key Players
Beyond CGRP: Exploring the Role of Substance P
Substance P, a neuropeptide, plays a crucial role in nociception and pain transmission. Its involvement extends beyond the simple transmission of pain signals, influencing the perception and modulation of pain experiences. Understanding the intricate interplay between CGRP and substance P is vital for developing effective pain management strategies. This complex interaction further highlights the multifaceted nature of chronic pain conditions.
Substance P is released alongside CGRP in many nociceptive pathways. This co-release may contribute to the synergistic effects observed in pain signaling, where the combined action of both peptides amplifies the pain experience. Further research is needed to fully elucidate the precise mechanisms involved in this complex interplay.
The Impact of Neurotrophic Factors
Neurotrophic factors, such as nerve growth factor (NGF), play a significant role in neuronal survival, growth, and function. Their presence is crucial in maintaining the integrity of nociceptive pathways and regulating pain transmission. Dysregulation of neurotrophic factors can contribute to the development and persistence of chronic pain conditions.
The Contribution of Inflammatory Mediators
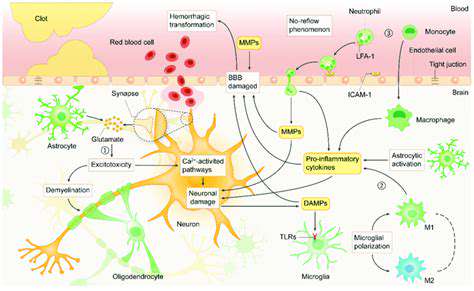
Inflammation is a complex biological response to harmful stimuli, often involving the release of various inflammatory mediators. These mediators, including cytokines and prostaglandins, can modulate nociceptive signaling and contribute to the development of chronic pain. Understanding the specific inflammatory mediators involved is crucial for developing targeted therapies to alleviate pain associated with inflammation.
Inflammation can persist even after the initial injury has healed, leading to a chronic state of pain. Targeting the inflammatory mediators involved in this process could be a promising avenue for pain management.
The Role of Ion Channels in Pain Transmission
Ion channels are essential components of neuronal membranes, controlling the flow of ions and ultimately influencing neuronal excitability and signal transmission. Specific ion channels, including voltage-gated sodium and calcium channels, are implicated in the initiation and propagation of pain signals. Disruptions in ion channel function can lead to altered pain perception and contribute to the development of chronic pain conditions. Understanding these ion channel mechanisms is key to developing more effective pain therapies.
The Importance of Central Sensitization
Central sensitization is a phenomenon where the central nervous system becomes more responsive to painful stimuli. This heightened responsiveness can lead to persistent pain even after the initial injury has healed. Factors contributing to central sensitization include altered synaptic plasticity and changes in neurotransmitter release in the central nervous system. Managing central sensitization is crucial for effective pain management in chronic pain conditions.
The Role of the Immune System in Chronic Pain
The immune system plays a more complex role than previously thought in chronic pain conditions. Immune cells can release various substances that modulate nociception and contribute to the development of pain. Understanding the interplay between the immune system and the nervous system in chronic pain is vital for developing more effective treatment strategies. The immune system's involvement is a significant advancement in the understanding of chronic pain mechanisms.
Disclaimer: All articles on this site are original, please do not reprint