Catalog
Excessive tension in the neck muscles is a common culprit of occipital pain.
Migraine attacks may produce radiating pain in the occiput.
Cervical disc herniation can trigger referred head pain.
Psychological stress may manifest as physiological headache symptoms.
Intracranial infections may cause intense throbbing pain in the occiput.
Visual fatigue often leads to associated tension in the muscles around the eyes.
Accurate identification of symptoms is the crucial first step in diagnosis.
Imaging examinations can clearly present abnormalities in tissue structure.
Customized rehabilitation training can effectively alleviate chronic pain.
Rational use of medication can quickly control acute symptoms.
Traditional Chinese medicine offers supplementary solutions to conventional treatments.
Adjusting daily routines is critical for long-term rehabilitation.
Persistent pain should consider the possibility of surgical treatment.
Sudden severe pain must be addressed with immediate medical attention to rule out risks.
Persistent pain affecting daily life requires professional assessment.
History of underlying diseases can significantly influence treatment plan choices.
Common Triggers for Pain in the Occipital Region
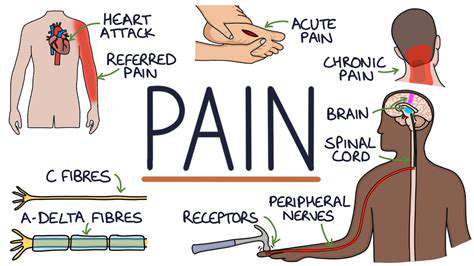
Muscle Strain and Poor Posture
The most common trigger for occipital pain in modern individuals is muscle strain in the neck and shoulders. Especially when working long hours at a desk, many people unconsciously lean their heads forward, which places an additional pressure of over 5 kilograms on the cervical spine. I have a patient who is a programmer and spends 12 hours a day in front of a computer; as a result, the muscles at the back of the head feel as hard as a rock, and the pain caused by chronic strain often spreads from the back of the neck to the entire occipital area.
In addition to occupational factors, improper sleeping posture can also cause problems. A lady I saw last week developed unbearable pain at the back of her head due to switching to a pillow that was too high. This situation can usually be significantly alleviated within 3-5 days through heat therapy and positional adjustments.
Special Manifestations of Migraine
Many people think migraines only occur at the temples, but nearly 30% of patients report their main pain point is in the area of the occipital nerve distribution. This type of pain often accompanies visual auras; a young patient described suddenly seeing jagged flashes in front of her eyes, followed by her occiput feeling as if it had been electrocuted. It is worth noting that this type of headache responds poorly to common pain relievers and requires specific medication treatment.
Recent studies have found that certain foods such as aged cheese and tyramine in red wine may trigger this type of headache. It is recommended that susceptible individuals keep a headache diary, noting dietary and activity details in the 24 hours leading up to an attack, as this can be particularly helpful in identifying triggers.
Chain Reactions from Cervical Pathology
- C4-C5 disc herniation may compress the greater occipital nerve.
- Bone spurs in the vertebrae can lead to insufficient blood supply to the vertebral artery.
- Joint dysfunction can cause protective muscle spasms.
Last week, while providing traction therapy for a cervical spondylosis patient, he was surprised to find that the pressure sensation at the back of his head immediately decreased by a third. This indicates a direct connection between cervical issues and occipital pain. Particularly for those who frequently look down, a straightening of the cervical curvature can lead to chronic pressure on nerve and blood vessels. It is advised that such patients perform a set of 'rice character exercises' every hour, which can effectively alleviate neck stiffness.
Somatic Manifestations of Psychological Stress
Anxiety disorder patients often complain of a tight feeling in the back of the head; this type of pain is characterized by its persistent presence from morning to night, yet physical exams fail to reveal any organic changes. A high school student I treated experienced such intense occipital pain due to pre-exam stress that he could not concentrate. After psychological counseling combined with relaxation training, his symptoms improved significantly.
These patients also exhibit a characteristic: the severity of pain is closely related to emotional fluctuations. It is recommended to try progressive muscle relaxation techniques, tightening and relaxing each body part starting from the toes, with the entire process taking about 20 minutes, which has proven effective in relieving tension-type headaches.
Infectious Diseases as Warning Signals
It is crucial to be particularly cautious, as sudden severe pain in the occiput may be a precursor to meningitis. Last year in the emergency department, I encountered a case where the patient initially experienced dull pain at the back of the head, which developed within 12 hours into projectile vomiting and stiff neck; lumbar puncture confirmed bacterial meningitis. This type of pain is often accompanied by high fever and worsens significantly at night, necessitating immediate medical intervention.
Even a simple common cold should not be taken lightly. Severe sinusitis may lead to purulent secretions irritating the meninges through anatomical pathways, provoking reflex headaches. It is advised to conduct a CT scan of the sinuses as soon as yellow-green nasal discharge appears alongside occipital pain.
The Subtle Impact of Visual Fatigue
Many people are unaware that an improper prescription for reading glasses can also cause occipital pain. The eye muscles must continuously strain to compensate for blurry vision, and this tension can transmit through the fascial chain to the occipital muscle groups. One patient tried three different pairs of reading glasses without resolution, only to discover that the underlying cause was visual fatigue from latent strabismus.
Long-term eye users should adopt the 20-20-20 rule: every 20 minutes, look at an object 20 feet away for 20 seconds. Combined with acupressure around the eyes (Jingming, Zuanzhu, Taiyang), this can effectively prevent headaches triggered by visual fatigue.
Key Diagnostic Points for Occipital Pain
Analysis of Symptoms' Temporal and Spatial Features
During diagnosis, it is essential to clarify the pain pattern: is it a persistent dull ache or episodic sharp pain? Is it worse in the morning and better in the evening, or stable throughout the day? A typical case involved a patient who experienced pounding pain at the back of the head only when lying flat; this was eventually diagnosed as obstruction of the internal jugular vein flow. This positional feature provided crucial clues for diagnosis.
Accompanying symptoms should also be noted. For example, dizziness along with occipital pain may indicate insufficient blood supply to the vertebrobasilar artery, while tinnitus may suggest a condition affecting the cranio-cervical junction. Patients are advised to prepare a symptom checklist prior to consultation, detailing attack frequency, duration, and factors that alleviate or exacerbate symptoms.
Imaging Examination Selection Strategies
For headaches persisting for more than 4 weeks, MRI scans can clearly reveal soft tissue abnormalities. However, it should be noted that patients over 40 should additionally undergo MRA to rule out vascular malformations. Last week, there was a case where the CT report was normal, but MRI revealed a meningioma of the cerebellar tentorium, indicating that the choice of examination method directly impacts diagnostic accuracy.
Special position X-rays can also be highly valuable. For example, a dance instructor experienced increased pain while leaning back, and dynamic imaging showed instability at C1-C2, a type of dynamic stability issue that is easily missed on routine MRI. Thus, clinical reasoning should not solely rely on imaging reports, but must integrate physical examination and holistic judgment.
Personalized Treatment Plan Analysis
Modern Advances in Physical Therapy
Fascial release techniques combined with neural gliding exercises have shown significant effects. The therapist first relaxes the suboccipital muscle groups manually and then guides the patient in performing self-directed neural gliding exercises. One patient who adhered to the treatment for 8 weeks reduced the frequency of headaches from 5 times a week to just 1 time a month.
New therapeutic equipment is also worth paying attention to. For instance, focused shockwave therapy can precisely target trigger points, and combined with deep heat therapy, it can improve local blood circulation. However, it should be noted that during the acute inflammation phase, heat therapy should be avoided, as it may exacerbate swelling.
The Art of Medication Use
For acute episodes, naproxen sodium is more effective than ibuprofen for pain relief, as it can inhibit both the COX-1 and COX-2 pathways. However, long-term use requires the addition of gastric mucosal protectants. For a patient with a history of peptic ulcers, we opted for topical diclofenac gel combined with oral omeprazole, ensuring efficacy while preventing gastrointestinal bleeding risks.
For preventive medication, topiramate is particularly effective for chronic tension-type headaches. However, it should be noted to gradually increase the dose, starting at 25mg at bedtime, increasing by 25mg each week, with a target dose of 75-100mg per day. Abrupt discontinuation may provoke seizures; strict adherence to medical advice is necessary.
The Wisdom of Traditional Chinese Medicine
When selecting acupuncture points, Fengchi and Kunlun points are particularly effective for occipital nerve pain. One patient felt an immediate sensation of the pain area melting like ice as soon as the needle was inserted at the Fengchi point. Combined with bloodletting cupping therapy, this method can quickly relieve muscle spasm states.
Herbal steaming is also worth trying. After boiling herbs such as Chuanxiong, Baizhi, and Qianghuo, the steam is used to invigorate the neck and cervical region, allowing the herbal vapors to penetrate the skin directly to the affected area. After 10 treatments, one patient reduced their headache severity from a VAS score of 8 to 3, and their sleep quality also significantly improved.
Details of Lifestyle Management
Office workers are advised to adjust their monitors to eye level and use ergonomically designed chairs. A patient who switched to a height-adjustable desk reported that alternating between standing and sitting each hour led to noticeable reduction in the bulge at the back of their neck and halved the frequency of headache attacks.
Adjusting sleeping positions can yield immediate results. It is recommended to place a pillow between the knees when sleeping on one side and to use a cylindrical support under the neck when sleeping on the back. A patient who switched to a memory foam wave pillow reported that the heaviness in the back of the head completely disappeared upon waking.
Criteria for Determining the Right Time to Seek Medical Attention
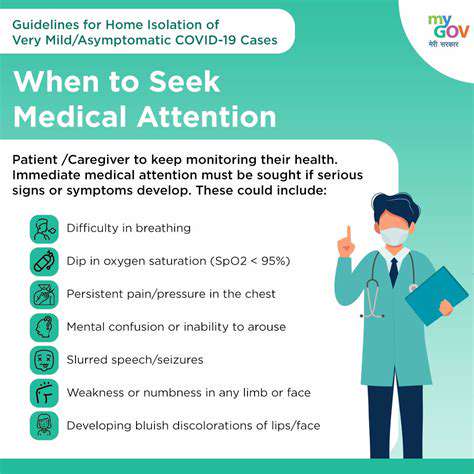
Recognition of Red Alert Signals
- Sudden thunderclap headache (reaches peak within 1 minute)
- Accompanied by changes in consciousness or limb numbness
- Fever accompanied by neck stiffness
Last year, I resuscitated a patient with a ruptured aneurysm. Their typical presentation was sudden explosive occipital pain, with CT showing subarachnoid hemorrhage. The severity of this pain surpassed any prior head pain experiences and requires immediate emergency response.
Another easily overlooked signal is pain that worsens with coughing. This may indicate increased intracranial pressure, commonly seen in venous sinus thrombosis or space-occupying lesions. Particularly in cases where headaches occur in the morning accompanied by projectile vomiting, there is a high suspicion of brain tumors.
Management Milestones for Chronic Pain
When headaches occur more than 15 days a month and last for over 3 months, it meets the diagnostic criteria for chronic daily headaches. At this point, simple pain relief may result in a vicious cycle, necessitating the initiation of a preventive treatment plan. One patient successfully reduced their headache days from 28 days per month to 5 days per month through cognitive behavioral therapy combined with medication.
If treatment effects plateau, it is also crucial to have follow-up consultations in a timely manner. For example, one patient showed significant progress during the first 3 weeks of physical therapy, but stagnated in the 4th week; adjusting the plan to include vestibular rehabilitation improved their condition again. This shows that treatment needs to be dynamically adjusted and should not remain fixed.
Special Considerations for Certain Populations
Pregnant women experiencing occipital pain should be especially cautious of preeclampsia. One expectant mother at 32 weeks believed she was experiencing just a common headache, only for her blood pressure to reach 170/110mmHg; an emergency cesarean section was subsequently performed to ensure the safety of both mother and child. It is advised that blood pressure be measured at every prenatal check-up after 20 weeks, especially for those with a family history.
Childhood headaches require particular caution. If school-age children complain of occipital pain accompanied by vomiting, intracranial infections should be ruled out first. A 7-year-old patient I treated experienced unsteady gait after 3 days of headache, and MRI confirmed cerebellitis; timely treatment prevented long-term sequelae.