The Nature of Pain and Its Impact on Life
The Biological Basis of Pain
Pain is a complex physiological response that involves various systems in the body, primarily the nervous system. Understanding the biological mechanisms of pain can aid in better treatment options. The sensation of pain typically begins when nociceptors, specialized pain receptors, are activated by harmful stimuli.
Once these receptors are triggered, they send signals through peripheral nerves to the spinal cord and then to the brain, leading to the perception of pain. This intricate signaling pathway highlights the body's immediate reaction to potential harm.
Moreover, the processing of pain is not just a single point event; it can be influenced by factors such as emotional well-being and psychological state. This intricate interplay means that pain is as much a psychological experience as it is a physical one.
The Psychological Dimension of Pain
The experience of pain transcends the physical realm and often intertwines with emotional states. Individuals living with chronic pain frequently report feelings of anxiety, depression, and social isolation. The psychological impact of pain can be profound, affecting overall quality of life.
Furthermore, the brain's interpretation of pain signals can vary significantly from person to person. Factors such as previous experiences, cultural background, and personal beliefs can all influence how pain is perceived and managed.
Coping strategies, which may include cognitive-behavioral therapy or mindfulness practices, can help individuals alter their relationship with pain. By addressing both psychological and physiological aspects, comprehensive pain management becomes more attainable.
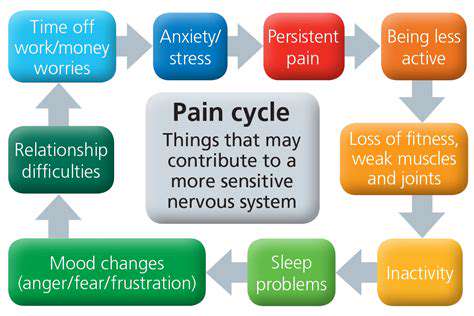
Chronic Pain and its Implications
Chronic pain is defined as pain that persists beyond the normal healing time, often lasting for months or even years. This condition not only diminishes physical functioning but also imposes significant emotional, financial, and social burdens on individuals.
The implications of chronic pain extend to various domains of life, affecting work productivity, relationships, and daily activities. As such, individuals may find themselves navigating a myriad of challenges, including stigma and misunderstanding from others.
Research continues to explore effective treatments and therapies for chronic pain management, emphasizing the need for a multidisciplinary approach. By integrating medical, psychological, and lifestyle strategies, those suffering from chronic pain can find pathways to improved well-being.
Types of Pain and Their Underlying Mechanisms
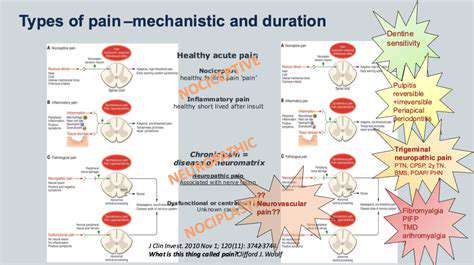
Understanding Nociceptive Pain
Nociceptive pain is the body's natural response to harmful stimuli, such as injury or inflammation. It serves a crucial protective function, alerting individuals to potential damage.
This type of pain is often categorized into somatic and visceral pain. Somatic pain originates from skin, muscles, and joints, while visceral pain arises from internal organs, illustrating the complexity of bodily responses to injury.
Exploring Neuropathic Pain
Neuropathic pain is distinct from nociceptive pain as it results from damage to the nervous system itself. Conditions such as diabetes or multiple sclerosis can lead to this type of pain, characterized by its burning or tingling sensations.
Understanding neuropathic pain is critical for developing effective treatment strategies. Patients often report challenges in managing this pain, highlighting the need for targeted therapeutic approaches.
The Impact of Psychological Factors on Pain Perception
Psychological factors play a significant role in how pain is perceived and experienced. Anxiety, depression, and stress can amplify the sensation of pain, making it feel more intense than it is physically.
This interplay between emotional and physical pain emphasizes the need for a holistic approach to pain management. Addressing psychological health, alongside physical treatments, can improve outcomes for patients suffering from chronic pain.
The Psychological Aspect of Pain Perception
The Role of Fear and Anxiety
Fear and anxiety can significantly amplify pain perception. When individuals are fearful of pain or anxious about their conditions, their brain's response to pain signals may heighten. This increased sensitivity can lead to a vicious cycle where pain reinforces fear and anxiety, further exacerbating the experience of discomfort.
Studies have shown that patients with chronic pain conditions often report elevated levels of fear. This fear can stem from previous painful experiences or a lack of understanding about their condition. As a result, even mild forms of discomfort can be perceived as more intense, leading to increased emotional distress.
Moreover, the anticipation of pain can also trigger a stress response in the body, releasing hormones that may intensify pain perception. This phenomenon underlines the importance of addressing psychological factors in pain management to help break this cycle.
Therefore, techniques such as cognitive-behavioral therapy, mindfulness, and relaxation strategies can be essential tools in reducing fear and anxiety. By changing the way individuals perceive and respond to pain, these approaches can improve overall pain management outcomes.
The Impact of Past Experiences
Past experiences with pain play a crucial role in shaping an individual's perception of future pain. If someone has endured significant pain in the past, their brain may become more attuned to signaling pain in similar situations, a phenomenon known as "pain sensitization." This can lead to a heightened response to pain even in the absence of any pathological cause.
Additionally, traumatic experiences related to pain can provoke a conditioned response, where the body reacts strongly to pain-related cues due to previous trauma. This can lead to an exaggerated sense of impending doom when facing situations reminiscent of those painful encounters.
Research indicates that individuals with a history of traumatic injuries or illnesses often report higher levels of pain intensity. As pain is not merely a physical sensation but intertwined with memory and emotion, understanding this relationship is vital for effective pain management strategies.
By exploring and addressing these past experiences through therapy or counseling, individuals can reframe their understanding of pain, which can diminish the fear and disablement that often accompany it.
The Importance of Social Support
Social support can substantially affect pain perception and coping strategies. Individuals who feel supported by family, friends, or peers often report lower levels of pain and improved coping mechanisms compared to those who feel isolated. Emotional support can buffer the effects of pain and create a more positive outlook on recovery processes.
Moreover, support groups provide spaces where individuals can share their experiences and coping strategies. Engaging with others facing similar challenges can foster a sense of belonging and reduce feelings of loneliness and despair, which can be particularly beneficial for those dealing with chronic pain.
Research suggests that social relationships can influence pain outcomes by providing emotional comfort and practical assistance. This can lead to enhanced resilience and a greater sense of control over one’s pain experience.
Encouraging open dialogue about pain within families and social circles is essential. Understanding the importance of connection can empower individuals to seek help when they need it and promote a stronger support network, ultimately improving their quality of life.
Social Factors Impacting Pain Management
Understanding the Role of Social Support
Social support plays a critical role in how individuals experience and manage pain. Support from family, friends, and caregivers can provide emotional comfort and practical assistance, resulting in better coping strategies.
Research suggests that patients with strong social networks often report lower levels of pain and better pain management outcomes. The presence of understanding and empathetic individuals can significantly alter a person's pain perception.
Conversely, social isolation can exacerbate feelings of pain and discomfort. Individuals lacking robust support systems may struggle more with both the physical and emotional challenges of pain, leading to a cycle of increased suffering.
The Impact of Socioeconomic Status
Socioeconomic status (SES) is a fundamental determinant of health and well-being that significantly influences pain management. Individuals from lower SES backgrounds may have limited access to healthcare resources, which can result in inadequate pain treatment.
Financial constraints often prevent people from seeking timely medical intervention, leading to a deterioration of their condition. Additionally, the stress associated with financial instability can heighten sensitivity to pain.
On the other hand, those with higher SES typically have better access to healthcare services, more informed healthcare choices, and greater advocacy for their needs, which can improve pain management experiences.
Cultural Perspectives on Pain
Cultural beliefs and attitudes towards pain can shape how individuals perceive and express their discomfort. Different cultures have unique methods for interpreting pain, which can affect the willingness to seek medical help and the types of treatments pursued.
For instance, in some cultures, pain may be viewed as a natural part of life, leading individuals to endure rather than seek relief. In contrast, other cultures might emphasize proactive pain management and open discussions about discomfort.
Healthcare providers must be culturally competent to offer effective pain management strategies. Understanding cultural backgrounds can aid in tailoring approaches that respect patients' beliefs while addressing their pain effectively.
The Influence of Environment on Pain Perception
The environment in which a person lives can have a considerable impact on their experience of pain. Factors such as housing conditions, community safety, and access to recreational activities all contribute to an individual’s overall mental and physical health.
An unsafe or stressful environment can elevate stress levels, which may aggravate pain symptoms. Conversely, a supportive and peaceful environment can promote healing and reduce the perception of pain.
Additionally, access to green spaces and recreational facilities can encourage physical activity, which is known to enhance pain management. Creating environments that foster well-being is essential in addressing the multifaceted nature of pain.
Innovative Approaches to Pain Relief

Integrative Therapies in Pain Management
Integrative therapies have emerged as a holistic approach to pain relief, recognizing that pain is not solely a physical phenomenon but also encompasses emotional and psychological dimensions. This multi-faceted perspective allows for tailored treatments that address the unique needs of each individual. Techniques such as acupuncture, massage therapy, and meditation can complement traditional medical treatments. Research indicates that these non-pharmacological methods can significantly reduce pain perception and enhance overall well-being.
An increasing number of healthcare providers are incorporating these integrative practices into standard care protocols. Patients often report improved satisfaction with their treatment programs when such therapies are included. By adopting a comprehensive approach, practitioners aim to enable patients to manage their pain effectively with fewer side effects.
Furthermore, integrative therapies promote patient empowerment, encouraging individuals to take an active role in their recovery. Educational programs that focus on self-care strategies, such as mindfulness or gentle yoga, can provide valuable tools for coping with pain. This shift towards self-management is crucial in fostering a sustainable approach to pain relief.
Notably, ongoing research continues to explore the effectiveness of these therapies. Emerging studies demonstrate significant potential for combining traditional and holistic methodologies. The evolving landscape of pain management continues to prioritize patient-centered care, aiming for optimal relief through diverse approaches.
Ultimately, the growing emphasis on integrative therapies highlights the necessity for a more nuanced understanding of pain. By bridging conventional medicine with alternative practices, we can pave the way for more effective and empathetic pain management solutions.
Technological Innovations in Pain Relief
Advancements in technology have revolutionized the field of pain relief, enabling more effective treatment modalities that were previously unimaginable. From wearable devices that track pain patterns to virtual reality environments designed for distraction, technology is reshaping pain management. These innovations not only enhance the patient experience but also provide healthcare professionals with valuable data for better treatment outcomes.
Neurostimulation devices, such as spinal cord stimulators, have shown significant promise in managing chronic pain. These devices work by sending electrical impulses to the spinal cord, helping to modify pain signals before they reach the brain. Patients equipped with such technology often report substantial reductions in pain and improved quality of life.
Another notable development is the use of telemedicine for pain management consultations. This approach facilitates access to specialists, especially for individuals in remote areas. By leveraging technology, patients can receive timely advice and support without the barriers of travel, thus enhancing adherence to treatment plans.
Artificial intelligence is also playing a pivotal role in pain management by analyzing vast amounts of data to predict pain flare-ups and recommend personalized treatment strategies. With continuous learning algorithms, AI holds the potential to identify patterns that may not be apparent to human practitioners. This dynamic capability can lead to more precise interventions tailored to individual patient needs.
In conclusion, the intersection of technology and healthcare is transforming pain relief strategies. As innovations continue to emerge, the potential for reducing pain, improving functionality, and enhancing the overall quality of life becomes increasingly promising. The integration of technology in pain management represents a significant advancement in our approach to tackling one of healthcare's most challenging issues.