Types of Common Analgesics
1. Non-Opioid Analgesics
Non-opioid analgesics are commonly used for mild to moderate pain relief. These medications are often available over the counter (OTC) and include options like acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen.
Acetaminophen is known for its effectiveness in reducing pain and fever. Unlike NSAIDs, it does not have anti-inflammatory properties, making it suitable for conditions where inflammation is not a primary concern. However, care should be taken to adhere to dosage guidelines to prevent liver damage.
NSAIDs work by inhibiting enzymes involved in the inflammatory process, thus providing pain relief as well as reducing inflammation and fever. While effective, there are potential side effects such as gastrointestinal irritation and increased risk of cardiovascular problems, especially when used long-term.
2. Opioid Analgesics
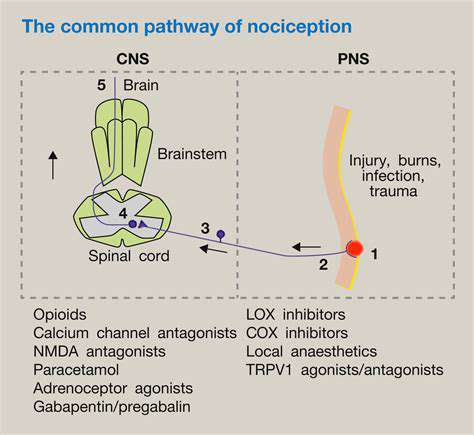
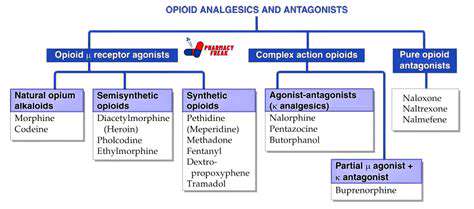
Opioid analgesics are potent pain-relieving medications that are generally used for moderate to severe pain. They are available by prescription and include drugs like morphine, oxycodone, and hydrocodone. These medications work by binding to specific receptors in the brain and spinal cord to diminish the perception of pain.
While opioids can be highly effective for short-term pain management, their use comes with significant risks, including the potential for addiction, tolerance, and respiratory depression. Thus, they are typically reserved for severe pain situations or cases where other analgesics are ineffective.
Patients prescribed opioids should be closely monitored by healthcare providers, and should also be educated on the signs of misuse and the importance of adhering to prescribed dosages to mitigate risks associated with these medications.
3. Adjunct Analgesics
Adjunct analgesics are medications that, while not primarily designed for pain relief, can enhance the effects of other analgesics or are effective for certain types of pain syndromes. This category includes antidepressants and anticonvulsants, which are often used in managing neuropathic pain.
Antidepressants like amitriptyline and duloxetine can help alleviate chronic pain conditions such as fibromyalgia and neuropathy. They work by altering pathways in the brain that influence pain perception, thereby providing relief to patients who may not respond to traditional pain medications.
Anticonvulsants, such as gabapentin and pregabalin, are also effective for nerve pain and are often incorporated into a pain management regimen for conditions like postherpetic neuralgia or diabetic neuropathy. These medications can reduce the frequency and severity of pain episodes when used alongside other analgesics.
1. Non-Opioid Analgesics
Understanding Non-Opioid Analgesics
Non-opioid analgesics are a critical component of pain management for many individuals. They provide relief from mild to moderate pain and are often the first line of treatment recommended by healthcare professionals.
These medications include common options like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen. Understanding their mechanisms of action can help patients select the right drug for their specific pain conditions.
Non-opioid analgesics are generally considered safer than opioids because they carry a lower risk of addiction and dependence. However, it is essential to use them according to prescribed guidelines to avoid side effects, such as gastrointestinal issues or liver damage.
Uses and Efficacy of Non-Opioid Analgesics
Non-opioid analgesics are particularly effective in treating conditions like headaches, arthritis, and muscle pain. They can also be beneficial for managing pain post-surgery or following an injury.
The efficacy of these medications often depends on the type and severity of the pain being treated. For instance, NSAIDs are excellent for pain with an inflammatory component, while acetaminophen might be preferred for general pain relief.
Patients should consult their healthcare provider to determine the most suitable non-opioid analgesic based on their medical history and specific pain situation, ensuring optimal results and minimizing risks.
Potential Side Effects and Precautions
While non-opioid analgesics are commonly used and considered safe, they are not without side effects. Frequent or high-dose use can lead to gastrointestinal bleeding or ulcers, particularly with NSAIDs.
Acetaminophen, on the other hand, poses risks to liver health, especially when taken in combination with alcohol or used excessively. Regular monitoring and adherence to recommended dosages can help mitigate these risks significantly.
Patients should always inform their healthcare providers about all medications they are taking, including over-the-counter drugs, to avoid potential interactions and ensure safe pain management.
2. Opioid Analgesics
2.1 Overview of Opioid Analgesics
Opioid analgesics are a class of medications that are primarily used to treat moderate to severe pain. They work by binding to specific receptors in the brain and spinal cord, leading to a reduction in the perception of pain. This mechanism makes them particularly effective for acute pain following surgery or injury, as well as for chronic pain conditions. Common examples include morphine, oxycodone, and hydrocodone.
While opioids can provide significant relief, they are also associated with various risks and side effects. One of the most concerning issues is the potential for addiction and abuse, which has become a major public health crisis in many countries. As a result, healthcare providers must carefully weigh the benefits and risks before prescribing these medications.
Opioids may also cause side effects such as sedation, constipation, and respiratory depression, which can complicate their use. Patient education is crucial to ensure that individuals understand how to use these medications safely and effectively. Monitoring patients for signs of misuse or dependence is also an essential aspect of opioid therapy.
In recent years, there has been a shift towards using opioid analgesics more judiciously. This includes exploring alternative methods for pain management, such as non-opioid medications, physical therapy, and integrative approaches. Such strategies aim not only to mitigate pain but also to minimize the risks associated with opioid use.
2.2 Clinical Guidelines for Opioid Use
Clinical guidelines for prescribing opioid analgesics emphasize a patient-centered approach. Physicians are encouraged to conduct a thorough assessment of each patient’s pain and overall medical history before initiating opioid therapy. These guidelines stress the importance of considering non-opioid alternatives wherever possible. When opioids are deemed necessary, starting with the lowest effective dose is advised to minimize the potential for side effects.
Documentation is another key element of opioid prescribing. Maintaining detailed records of the patient's pain levels, treatment response, and any adverse effects can help healthcare providers adjust treatment as needed. Regular follow-up appointments are strongly recommended to reassess pain management strategies and ensure the patient’s well-being.
In addition, many guidelines suggest incorporating risk assessment tools to evaluate a patient’s likelihood of misuse or addiction, which can inform medication choices and monitoring protocols. Providing clear expectations and guidelines for opioid use can also empower patients to be active participants in their pain management.
As the opioid crisis continues to evolve, ongoing education for healthcare providers about safe prescribing practices is essential. This includes staying updated on the latest evidence-based research and state regulations regarding opioid prescribing, ensuring that providers can offer effective and responsible pain management options to their patients.
Considerations for Safe Use
Understanding the Types of Analgesics
Analgesics, commonly referred to as pain relievers, can be categorized into two main types: non-opioid and opioid analgesics. Non-opioids, such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), are often used for mild to moderate pain relief. These medications work by inhibiting the body's production of prostaglandins, which are chemicals that promote inflammation and pain sensation.
Opioid analgesics, including morphine, hydrocodone, and oxycodone, are typically prescribed for more severe pain, such as that associated with surgery or cancer. They act on opioid receptors in the brain to block the perception of pain, but they come with a higher risk of dependency and side effects, making their use more controversial and strictly regulated.
Dosage and Administration Guidelines
Safe use of analgesics requires adherence to recommended dosages and administration guidelines. For over-the-counter analgesics, it's essential to read the label carefully to avoid exceeding maximum daily doses, which can lead to serious health issues like liver damage with acetaminophen or gastrointestinal bleeding with NSAIDs.
Prescription analgesics must be used strictly according to a healthcare provider's instructions. Patients should ensure they understand the dosing schedule, potential side effects, and the importance of not mixing these medications with alcohol or other substances that can exacerbate adverse effects.
Potential Side Effects and Interactions
While analgesics can provide significant relief, they are not without potential side effects. Common side effects of non-opioid analgesics include nausea, stomach upset, and increased risk of heart problems with extended use of NSAIDs. Opioids can cause more severe side effects, including sedation, constipation, and the risk of overdose, especially if taken in higher amounts than prescribed.
Additionally, some medications can interact with analgesics, altering their effectiveness or increasing the risk of adverse effects. For example, combining NSAIDs with blood thinners can increase bleeding risks, while using opioids with benzodiazepines can lead to life-threatening respiratory depression. Always consult a healthcare provider before starting any new medications.
Special Considerations for Vulnerable Populations
Certain populations may require special consideration when it comes to the use of analgesics. Elderly patients often have greater sensitivity to medications and may be at higher risk for side effects due to slower metabolism and prevalence of multiple health conditions. Therefore, their pain management plans should be tailored to minimize risks while still providing adequate relief.
Patients with pre-existing conditions, such as liver or kidney disease, should also consult their healthcare providers regarding the safest analgesic options. In some cases, alternative therapies like physical therapy or acupuncture may be recommended as adjunct treatments to medication.
Alternative Pain Management Strategies
In addition to traditional analgesics, various alternative pain relief strategies can enhance overall treatment effectiveness. Mindfulness meditation, yoga, and cognitive-behavioral therapy are increasingly recognized for their ability to help patients manage pain through mental and emotional techniques.
Physical therapies, such as massage, chiropractic care, and exercise, can also play a critical role in pain management. These methods may help to strengthen muscles, improve flexibility, and promote overall well-being without the risks associated with pharmacological treatments, making them suitable adjuncts to analgesic use.