Causes of Cervicogenic Headaches
Muscle Tension and Postural Issues
Cervicogenic headaches often arise from muscle tension in the neck and shoulder region. Poor posture, especially during prolonged periods of sitting or computer use, can contribute significantly to this tension.
This tension can lead to pain that radiates from the neck to the head, often mimicking tension-type headaches. Addressing ergonomic issues can help alleviate these symptoms and reduce headache frequency.
Injuries and Trauma
Injuries, particularly whiplash or other neck trauma, can be significant contributors to cervicogenic headaches. After an injury, the neck muscles and vertebrae may become irritated or misaligned, leading to pain that manifests as a headache.
Recognizing the connection between previous neck injuries and headache symptoms is crucial for effective treatment. Proper assessment and rehabilitation following such injuries can help prevent chronic headache development.
Degenerative Disc Disease
As people age, they may experience degenerative changes in the cervical spine, leading to conditions such as disc herniation or cervical spondylosis. These changes can irritate the surrounding nerves and tissues, resulting in cervicogenic headaches.
Early intervention and management of spinal health can reduce the impact of these degenerative conditions on overall well-being. Treatments may include physical therapy or lifestyle modifications aimed at maintaining spinal integrity.
Stress and Emotional Factors
Stress is another significant contributor to cervicogenic headaches, as it can lead to increased muscle tension in the neck and shoulders. Moreover, emotional factors such as anxiety or depression can exacerbate headache symptoms.
Implementing stress management techniques, such as mindfulness or relaxation exercises, can be beneficial in reducing headache severity. Addressing emotional health is just as important as physical treatment for effective headache relief.
Symptoms Associated with Cervicogenic Headaches
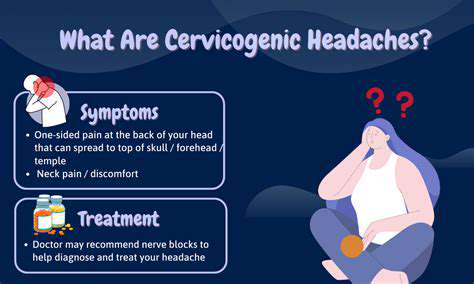
Common Symptoms of Cervicogenic Headaches
Cervicogenic headaches often present with a distinctive type of pain, which is typically unilateral and can be described as a dull, aching sensation. The pain may also radiate from the neck to the forehead, temples, or behind the eyes. This pattern can make it challenging to distinguish these headaches from other types, such as migraines or tension headaches.
In addition to pain, individuals may experience associated symptoms like stiffness in the neck, limited range of motion, and tenderness in the neck and shoulder muscles. These accompanying symptoms can often exacerbate the overall discomfort, leading to a reduced quality of life.
Some people with cervicogenic headaches might also have symptoms like visual disturbances, nausea, or even dizziness. Identifying these symptoms early on is crucial for effective diagnosis and management.
Identifying Triggers and Risk Factors
Understanding the triggers of cervicogenic headaches is essential for effective management. Common triggers include poor posture, repetitive neck movements, or even prolonged periods spent in front of a computer. These activities can strain the neck muscles and lead to the development of headaches.
Other risk factors may include previous neck injuries, such as whiplash, or underlying conditions like osteoarthritis. Identifying these risk factors can help in developing preventative strategies and treatment plans.
It’s also crucial to consider lifestyle factors, such as stress levels and sleep quality, which can significantly affect the frequency and intensity of headaches. Integrating lifestyle modifications may provide added relief and help in reducing the occurrence of cervicogenic headaches.
Treatment Options for Cervicogenic Headaches
Treatment Methods Overview
Cervicogenic headaches are often treated through a combination of approaches tailored to the individual’s needs. Choosing the right treatment plan can significantly reduce pain and improve quality of life. Healthcare providers may recommend various interventions ranging from physical therapy to medication. Understanding the complexities of these headaches is crucial in deciding the most effective treatment strategy.
The goal of treatment is to relieve pain and address the underlying musculoskeletal issues contributing to the headaches. Options can include manual therapy, stretching, and strengthening exercises. In some cases, it may also involve ergonomic assessments to modify activities that trigger headaches.
A comprehensive treatment plan often incorporates both passive treatments, such as heat or ice application, and active treatments, such as exercise. This multifaceted approach can lead to better long-term outcomes for patients suffering from cervicogenic headaches. Always consult a healthcare professional to explore the most appropriate methods for your situation.
Incorporating lifestyle modifications can also complement these treatments. Maintaining good posture, ensuring proper workstation ergonomics, and managing stress play important roles in alleviating symptoms.
Physical Therapy Techniques
Physical therapy is a cornerstone in the treatment of cervicogenic headaches. Therapists often use modalities like ultrasound or electrical stimulation to relieve pain. Manual therapy, including joint mobilization and manipulation, can improve neck function and reduce headache frequency.
Exercises focused on strengthening the neck and upper back muscles may also help reduce strain on the cervical spine. These exercises aim to enhance flexibility and support proper posture, which are vital in managing headaches. Regular physical therapy sessions can provide ongoing support and adjustment of treatment as needed.
Furthermore, education on body mechanics and posture can empower patients to take charge of their recovery. Learning how to properly engage in daily activities without straining the neck is crucial for long-term relief. True recovery comes from consistent practice and adherence to the techniques taught during therapy.
Physical therapists tailor their approach based on the individual’s symptoms and their response to treatment. As a result, each therapy plan can look different for each person, making a personalized approach effective in managing cervicogenic headaches.
Medications for Pain Relief
Medications can play a significant role in the acute management and prevention of cervicogenic headaches. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are often the first line of treatment. These medications can help to alleviate pain during headache episodes and make daily activities bearable.
In cases of more severe pain, healthcare providers may prescribe stronger medications or muscle relaxants. It's important for patients to closely follow their doctor’s instructions when using these medications to avoid potential side effects. Understanding the appropriate use of medications is vital for effective pain management.
Some patients may also benefit from preventive medications, such as antidepressants or medications that target nerve pain. These can be prescribed based on the frequency and severity of headaches. Regular follow-ups with a healthcare provider are essential to monitor medication effectiveness and make dosage adjustments as needed.
Combining medication with other treatment modalities, such as physical therapy, can enhance overall outcomes. It is vital to maintain open communication with healthcare providers about any side effects or changes in symptoms to ensure the best possible care.
Alternative Therapies and Lifestyle Modifications
In addition to conventional medical treatments, many patients explore alternative therapies to manage cervicogenic headaches. Acupuncture is one such option that some individuals find beneficial. This practice involves inserting thin needles into specific points on the body to relieve pain and restore balance.
Chiropractic care may also offer relief through spinal manipulation and adjustments. Many individuals report significant improvements in headache frequency and intensity after a series of chiropractic treatments. Incorporating such therapies can be an effective complement to traditional modalities.
Holistic approaches, including yoga and mindfulness meditation, can enhance relaxation and potentially reduce headache occurrences. Engaging in regular physical activity can also improve overall health and reduce stress, which may contribute to fewer headaches. Incorporating these lifestyle changes often leads to a more effective and well-rounded management plan.
It is important to approach alternative therapies with an open mind but also to consult healthcare professionals to ensure safety and efficacy. Each individual's response to these treatments may vary, so personalized assessments are essential in finding the right combination for headache relief.
When to Seek Professional Help
For individuals with cervicogenic headaches, understanding when to seek professional help can make a significant difference. If headache symptoms persist, worsen, or become chronic, it is crucial to consult a healthcare provider. Early intervention can prevent more severe complications and ensure timely management.
Additionally, if headaches are accompanied by other concerning symptoms such as vision changes, confusion, or weakness, immediate medical attention is necessary. These could be signs of more serious underlying issues requiring prompt assessment.
Regular check-ups with healthcare professionals can also help patients monitor progress and adjust treatment plans as needed. Staying proactive about healthcare can empower individuals to embrace effective lifestyle changes and treatment strategies.