Die Rolle von Mastzellen bei Kopfschmerzen
Mastzell-Aktivierungs-Syndrom (MCAS) und die Verbindung zu Kopfschmerzen
Das Mastzell-Aktivierungs-Syndrom (MCAS) ist eine komplexe Erkrankung, die durch die Überaktivierung von Mastzellen, spezialisierten Immunzellen im gesamten Körper, gekennzeichnet ist. Erkennen der Migräne-Symptome im Zusammenhang mit MCAS Kopfschmerzen können sich auf verschiedene Weise äußern, von einem dumpfen Schmerz bis zu einem Die Identifizierung spezifischer auslösender Faktoren ist entscheidend für die Behandlung von MCAS-bedingten Kopfschmerzen. Obwohl die Auslöser zwischen den einzelnen Personen stark variieren können, gehören häufig vorkommende Faktoren Lebensmittel, die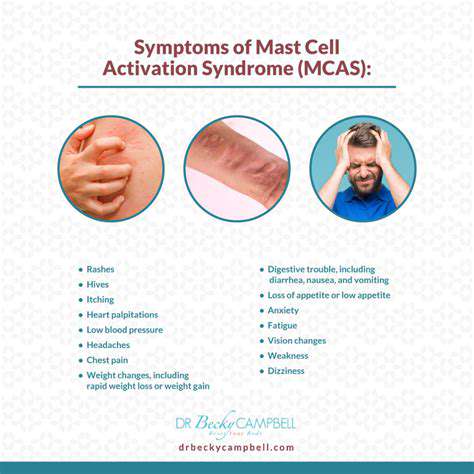
Verstehen der verschiedenen Arten von Kopfschmerzen
Auslösende Faktoren und Ernährungshinweise bei MCAS-bedingten Kopfschmerzen
Auslösende Faktoren bei MCAS-bedingten Kopfschmerzen
Diagnose und Managementstrategien suchen

Die Bedeutung einer frühen Diagnose verstehen
Read more about Mastzell-Aktivierungs-Syndrom (MCAS) und die Verbindung zur Kopfschmerzen
Wie Entzündungen Schmerzen Auslösen: Die Verborgene Verbindung
Mein Hals Tut Weh, Wenn Ich Den Kopf Drehe: Mögliche Ursachen
Die Bedeutung einer angemessenen Flüssigkeitsaufnahme für die allgemeine Gesundheit
Intimität und Beziehungen trotz chronischer Migräne erhalten
Aufbau der Selbstwirksamkeit: Vertrauen in Ihre Fähigkeit, Migräne zu bewältigen
Migräne-Aura jemandem erklären, der sie nicht erlebt hat
Rückprallkopfschmerzen vs. verschlimmernde Migräne: Wie man sie unterscheidet
Übersetzung von Migräneforschung in praktische tägliche Strategien
Eine Vision für Ihr Wohlbefinden jenseits der Migräne-Behandlung schaffen
Kopfschmerzen im Zusammenhang mit dem Temporomandibulargelenk-Syndrom (TMGS) verwalten
Wie der Klimawandel die Migräne-Muster weltweit beeinflussen könnte