Introduction to Headache Classification
Primary Headaches
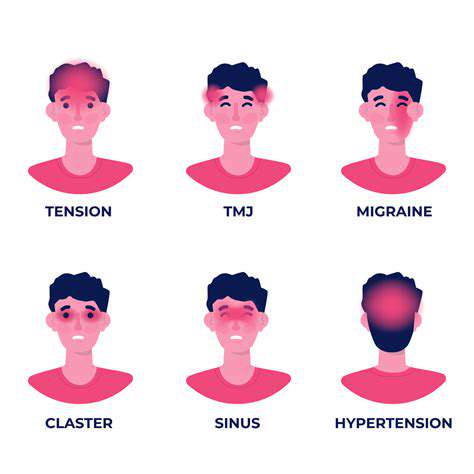
Primary headaches are not symptoms of an underlying disease but instead represent discrete conditions that can be classified into various types. The three most common types of primary headaches are tension-type headaches, migraines, and cluster headaches. Each type has its unique characteristics and triggers, making understanding them essential for effective treatment.
Tension-type headaches are characterized by a dull, aching pain that can feel like a tight band around the head. They are often triggered by stress, poor posture, or muscle tension and can last for hours or even days. While they are generally not severe, recurring episodes can significantly impact a person's quality of life.
Migraine headaches are more intense and often accompanied by symptoms such as nausea, vomiting, and sensitivity to light and sound. They can last from several hours to several days and are often preceded by warning signs known as aura. These can include visual disturbances, tingling sensations, or headache-related changes in mood.
Cluster headaches, although less common, are incredibly painful and typically occur in cycles or clusters. They usually affect one side of the head and are often accompanied by additional symptoms such as nasal congestion and watery eyes. These headaches can significantly disrupt daily activities, making it crucial for individuals to identify and manage their triggers effectively.
Secondary Headaches
Secondary headaches are indicative of an underlying health issue. Unlike primary headaches, these types arise as a symptom of another medical condition, such as an illness, trauma, or infection. Common causes of secondary headaches include sinus infections, head injuries, and conditions such as hypertension or strokes.
Sinus headaches, for example, are often associated with sinusitis and are characterized by pain and pressure around the forehead, cheeks, and eyes. Despite their common association with colds or allergies, it's essential to differentiate sinus headaches from other headache types to ensure appropriate treatment.
Additionally, headaches resulting from head injuries can range from mild to severe and may indicate serious complications like concussions. It is crucial to seek medical attention following any head trauma to rule out serious underlying conditions.
Other secondary headaches may arise from conditions like meningitis or encephalitis, which can be life-threatening and require immediate medical intervention. Identifying these headaches swiftly enhances the likelihood of effective treatment and minimizes potential complications, making awareness crucial for anyone suffering from recurring or intense headaches.
Primary vs. Secondary Headaches
Understanding Primary Headaches
Primary headaches are conditions that are not caused by any underlying disease. Instead, they are considered standalone disorders that can be triggered by various factors. Common types of primary headaches include tension-type headaches, migraines, and cluster headaches.
Tension-type headaches are the most prevalent form and often feel like a tight band around the head. These headaches can stem from stress, anxiety, or posture issues. They may also be episodic or chronic, depending on the frequency and duration of the episodes.
Migraines, on the other hand, are characterized by severe, throbbing pain typically on one side of the head. They can be accompanied by other symptoms such as nausea, vomiting, and sensitivity to light or sound. Understanding the triggers for migraines is vital for effective management, as they can include hormonal changes, certain foods, or environmental factors.
Cluster headaches are less common but extremely painful. They occur in cyclical patterns, leading to frequent headaches over weeks or months, followed by periods of remission. The exact cause of cluster headaches is not fully understood, but they often occur at the same time each day and can cause intense discomfort around one eye.
The Nature of Secondary Headaches
Secondary headaches arise as a symptom of another underlying condition. These can result from various medical issues, including infections, head injuries, or even more serious conditions like tumors or aneurysms. Understanding secondary headaches is crucial for proper diagnosis and treatment.
One of the most common causes of secondary headaches is sinus infection. The inflammation in the sinus cavities can lead to pain that may feel like pressure in the forehead, cheeks, and behind the eyes. Treatment often focuses on resolving the sinus infection itself.
Another example of a secondary headache is one that occurs after a head injury, including concussions. Post-trauma headaches can vary significantly in intensity and duration, and it is essential to consult a healthcare provider to evaluate the situation properly.
More severe causes of secondary headaches include conditions like meningitis or hypertension. Meningitis, an inflammation of the protective membranes covering the brain and spinal cord, can often present with a severe headache among other symptoms. Recognizing these secondary headaches and their potential severity is vital for timely medical intervention.
Tension-Type Headaches
Understanding Tension-Type Headaches
Tension-type headaches (TTH) are among the most common forms of headaches experienced by people of all ages. They are characterized by a dull, aching pain, often described as a tight band around the head. Unlike migraine headaches, TTH usually don't include symptoms such as nausea or sensitivity to light and sound.
Tension-type headaches can be episodic, occurring occasionally or sporadically, or they can become chronic, occurring on 15 or more days per month. While the exact cause of TTH is not fully understood, stress, poor posture, and muscle tension are believed to be significant contributors.
Proper understanding of TTH can help patients recognize patterns and symptoms, providing them with tools and strategies for effective management. Recognizing when a headache is tension-related can lead to better coping mechanisms and treatment options.
Causes and Triggers of Tension-Type Headaches
There are several factors that can lead to the development of tension-type headaches. Emotional stress, such as anxiety or depression, is one of the leading triggers. Additionally, physical factors like muscle strain due to poor posture or prolonged screen time can contribute significantly.
Other common triggers include fatigue, lack of sleep, dehydration, and skipping meals. Identifying personal triggers is crucial for those who suffer from recurrent tension-type headaches, as it allows them to take proactive measures to avoid these situations.
Additionally, environmental factors like noise, lights, and even temperature changes can provoke tension headaches. Keeping a headache diary can help individuals pinpoint their specific triggers and adjust their routines accordingly.
Symptoms Associated with Tension-Type Headaches
The primary symptom of tension-type headaches is a persistent, aching pain that may feel like pressure around the forehead or back of the head and neck. This pain is usually mild to moderate in intensity and is often bilateral, meaning it affects both sides of the head.
Other symptoms may include tenderness in the scalp, neck, and shoulder muscles. Individuals might not experience additional symptoms like nausea or vomiting, which distinguishes TTH from migraines.
Some individuals may also report tightness in the neck and shoulders, which can exacerbate the discomfort. It’s essential to recognize these symptoms early to implement effective management strategies.
Treatment Options for Tension-Type Headaches
There are various treatment options available for managing tension-type headaches. Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can be effective for alleviating mild symptoms. However, it is important for individuals to adhere to recommended dosages to avoid medication overuse headaches.
In addition to medication, lifestyle changes play a significant role in managing TTH. Regular exercise, maintaining proper hydration, and ensuring adequate sleep can help reduce the frequency and intensity of headache episodes.
Stress management techniques such as mindfulness, yoga, or meditation can also provide relief. Physical therapy may benefit those with muscle tension, while cognitive-behavioral therapy can help address the psychological aspects of stress-related headaches.
Preventative Strategies for Tension-Type Headaches
Preventative strategies are crucial for those prone to tension-type headaches. Establishing a consistent routine that includes regular meals, hydration, and sleep patterns can significantly reduce the likelihood of episodes.
Incorporating regular physical activity, including stretching and relaxation exercises, can promote muscle relaxation and help mitigate tension build-up. Setting regular breaks during activities that require prolonged focus, such as computer work, can also help.
Stress management techniques play a vital role in preventing TTH. Utilizing relaxation techniques, time management, and finding outlets for stress relief can empower individuals to take control over their headache frequency. Keeping a headache diary may assist in identifying patterns and incorporating effective strategies into daily life.
Migraines
Understanding Migraines
Migraines are a specific type of headache that are often characterized by intense, throbbing pain, usually on one side of the head. They can be accompanied by other symptoms such as nausea, vomiting, and extreme sensitivity to light and sound. These headaches can last anywhere from a few hours to several days, leading to significant disruption in daily activities.
Research suggests that migraines are caused by a combination of genetic, environmental, and neurological factors. Changes in brain chemistry, particularly involving serotonin, play a central role in the onset of migraines. Identifying triggers such as stress, hormonal changes, certain foods, and sleep disturbances can help individuals manage their migraine episodes more effectively.
There are various types of migraines, including migraine with aura and migraine without aura. Migraines with aura are preceded by visual or sensory disturbances, such as flashes of light or tingling in the limbs, while migraines without aura occur without these initial symptoms. Understanding the type of migraine can aid in developing a more effective treatment strategy.
Treatment options for migraines range from over-the-counter pain relief medications to prescription drugs specifically designed to treat migraines. Lifestyle changes, such as regular exercise, hydration, and a balanced diet, can also contribute to reducing the frequency and severity of migraine attacks.
Managing Migraines Effectively
Effective management of migraines often requires a comprehensive approach that includes both preventive measures and acute treatment options. Preventive treatments might involve daily medications prescribed by healthcare providers, aimed at reducing the frequency and intensity of migraine attacks.
In addition to medication, keeping a headache diary can be an invaluable tool for those suffering from migraines. By documenting the frequency, duration, and triggers associated with migraines, individuals can gain insights into patterns and potential causes of their headaches.
Alternative therapies, such as acupuncture, biofeedback, and cognitive-behavioral therapy, have also shown promise in helping individuals manage migraines. These methods can address both the physical and psychological aspects of migraines, providing a more holistic approach to treatment.
Furthermore, educating oneself about migraines and staying informed about the latest research and treatment options can empower individuals to take charge of their health. Consulting with healthcare professionals can also provide tailored strategies that take into account specific circumstances and preferences.
Cluster Headaches
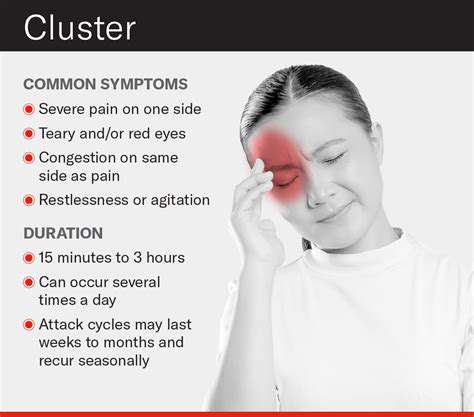
What Are Cluster Headaches?
Cluster headaches are one of the most intense types of primary headaches. They are characterized by severe pain, often described as a burning or piercing sensation. These headaches typically occur in cyclical patterns, known as clusters, which can last from weeks to months. During a cluster period, an individual may experience multiple headache attacks each day.
Cluster headaches primarily affect men, particularly those aged between 20 and 40. The exact cause of cluster headaches is still not completely understood, but they are believed to involve the hypothalamus, an area of the brain that regulates biological rhythms.
Symptoms often include a sudden onset of debilitating pain, usually on one side of the head, often around the eye. Individuals may also experience watering of the eye or nasal congestion on the affected side. The frequency and duration of these attacks vary considerably from person to person.
It is crucial for those experiencing such symptoms to consult a healthcare professional for an accurate diagnosis and appropriate treatment options. Early intervention can significantly improve quality of life during cluster periods.
While the exact mechanism of cluster headaches remains unclear, potential triggers can include alcohol, strong odors, and changes in sleep patterns.
Symptoms and Diagnosis
The hallmark of cluster headaches is the severe, unilateral pain that typically lasts between 15 minutes and three hours. Patients often describe the pain as excruciating, making it difficult to sit still during an attack. Associated symptoms can include redness and swelling around the eye, drooping eyelid, and restlessness.
The diagnosis of cluster headaches is primarily based on a patient's medical history and a detailed account of their symptoms. Healthcare providers may also perform imaging tests, such as a CT scan or MRI, to rule out other potential causes of headache.
Keeping a headache diary can be an effective way for patients to track the frequency, duration, and intensity of their headaches, as well as any potential triggers. This information can be invaluable in guiding treatment decisions.
In some cases, neurologists may utilize a specific criteria set by the International Classification of Headache Disorders to accurately diagnose cluster headaches. Understanding the patterns and predicting the onset of attacks is crucial for those living with this type of headache.
Ultimately, an accurate diagnosis leads to effective treatment, helping individuals manage their symptoms more successfully.
Treatment Options
Cluster headaches can be managed through a combination of acute and preventive treatments. Acute treatments aim to relieve pain during an attack, while preventive treatments are intended to decrease the frequency of attacks. Common acute treatments include oxygen therapy and triptans, which are medications specifically designed to treat migraine and cluster headaches.
For those suffering from chronic cluster headaches, preventive medications like corticosteroids, verapamil, and lithium may be prescribed. These medications require a careful assessment by a healthcare provider to determine the most appropriate regimen.
Additionally, certain lifestyle modifications can potentially help mitigate the intensity and frequency of cluster headaches. Avoiding known triggers, maintaining a regular sleep schedule, and minimizing alcohol consumption can make a significant difference.
Some patients find relief through alternative therapies, such as acupuncture or the use of melatonin supplements. Consulting with a healthcare provider about these options can help patients find a tailored approach that works for them.
Moreover, ongoing research into new treatments and therapies continues to provide hope for those affected by this debilitating condition.
Living with Cluster Headaches
Living with cluster headaches can be incredibly challenging, not just for the affected individual but also for their families. The sudden onset and unpredictability of the attacks can disrupt daily activities and routines. Support from family and friends is essential as it can provide emotional stability during difficult times.
Many people find it helpful to educate themselves about the condition and connect with others who share similar experiences. Online forums and support groups can offer valuable resources and a sense of community.
Stress management techniques, such as mindfulness and relaxation exercises, can also help. Individual coping strategies, whether through professional therapy or personal hobbies, can facilitate better management of the emotional toll of frequent headaches.
Keeping a positive mindset and developing a robust coping strategy are crucial for managing the emotional aspects of living with cluster headaches. Having a solid support system can enhance resilience and help individuals find joy amidst the pain.
In summary, although dealing with cluster headaches can be difficult, understanding the condition, seeking the right treatments, and staying connected with support networks can significantly improve quality of life.
Secondary Headaches
Understanding Secondary Headaches
Secondary headaches are those that arise as a symptom of another underlying health condition. They are not classified as standalone headaches but rather as signals that something else is occurring in the body. Identifying the root cause of secondary headaches is crucial for effective treatment.
Common conditions that can lead to secondary headaches include infections, brain injuries, and medications. For instance, conditions like sinusitis can lead to significant sinus pressure, resulting in headaches. This category encompasses a wide variety of potential triggers, making it essential to consult a healthcare provider.
Diagnosis often involves a thorough medical history and may include imaging tests to pinpoint the cause. Treatment typically focuses on addressing the underlying issue rather than treating the headache itself. Understanding this difference is vital for long-term relief.
Types of Secondary Headaches
There are several types of secondary headaches, each associated with different medical conditions. Cervicogenic headaches, for instance, are caused by issues in the neck, often related to poor posture or injury. These headaches can often be alleviated with physical therapy and appropriate treatment for the neck.
Other notable types include hormonal headaches, linked to fluctuations in hormone levels, particularly in women during their menstrual cycle or pregnancy. These headaches can be managed with hormonal therapy or lifestyle adjustments.
More severe types of secondary headaches include those caused by tumors or bleeding in the brain. Recognizing these types is vital, as they may require immediate medical intervention to prevent serious complications.
Symptoms and Warning Signs
The symptoms of secondary headaches can vary significantly depending on their origin. Typical symptoms may include a sudden onset of intense pain, changes in vision, or neurological symptoms such as weakness or difficulty speaking. Recognizing these symptoms early can be crucial for effective treatment.
In addition to pain, secondary headaches might be accompanied by other signs, such as fever or a stiff neck. These symptoms may indicate more serious conditions, such as meningitis or encephalitis, warranting immediate medical attention.
Monitoring the frequency, duration, and intensity of the headaches can also provide valuable information to healthcare providers in diagnosing the underlying cause. Keeping a headache diary might help track triggers and responses to treatment.
Treatment Options for Secondary Headaches
Treatment for secondary headaches focuses on addressing the underlying cause rather than just alleviating the headache itself. This may involve medication to treat an infection, physical therapy for neck issues, or lifestyle changes for hormonal imbalances. Pain relief medications might also be prescribed, but these should be used sparingly to avoid overuse headaches.
In cases of more severe conditions, such as tumors or structural issues within the brain, surgical interventions may be necessary. Consulting a specialist can provide specific insights into the most effective treatment options based on the headache's origin.
In addition to medical treatments, self-care strategies can significantly reduce the frequency and severity of secondary headaches. These may include stress management techniques, adequate hydration, and regular exercise to maintain overall health and well-being.