A Comprehensive Analysis and Coping Strategies for Side Head Pain
Common Pain Triggers Explained
Muscle Tension and Stress Responses
The common problem of neck stiffness among modern people often becomes the trigger for headaches. Prolonged fixed postures when using electronic devices cause continuous contractions of the trapezius and sternocleidomastoid muscles, leading to a sense of pressure on both sides of the head. Clinical data from the \Journal of Headache Medicine\ indicates that nearly two-thirds of workplace individuals experience recurrent headaches caused by stress-related muscle tension. This dull pain is particularly noticeable when pressing on the temples, resembling a tight headband.
It is important to note that long-term psychological stress can cause muscle memory contractions, creating a vicious cycle. It is recommended to try progressive muscle relaxation techniques: gradually tense and then relax muscle groups starting from the toes, with diaphragmatic breathing for better results. Swimming or yoga three times a week can significantly improve muscle coordination.
Neurological Abnormalities
During migraine attacks, patients often describe the sensation as if a power drill is pulsating in their temples. Statistics from the American Headache Society show that this type of neuropathic pain troubles 12% of the adult population, with the incidence in women being three times that of men. Typical symptoms include photophobia, nausea, and even visual auras—flashing zigzag lights in front of the eyes.
Although cluster headaches are rare, they are more intense, with patients often describing sensations similar to a burning iron piercing the eye socket. Keeping a detailed headache diary (noting the time of onset, duration, and triggers) can provide important diagnostic information for physicians. Recent research has found that medications that regulate serotonin levels combined with biofeedback therapy can reduce the frequency of attacks by more than 50%.
Infectious Foci Impact
Headaches caused by sinusitis exhibit a typical time pattern—most severe upon waking in the morning, gradually easing in the afternoon. Experts in otolaryngology point out that inflammation of the ethmoid and sphenoid sinuses often radiates to the temporal region, causing a pulsating pain sensation. If accompanied by yellow-green nasal discharge and facial tenderness, bacterial infection should be considered.
It’s noteworthy that odontogenic infections can sometimes masquerade as regular headaches. The author has treated a patient misdiagnosed for three months, ultimately discovering that a periapical abscess of the second molar led to referred pain. It is recommended that when persistent unilateral headaches occur, one should gently tap the teeth to rule out odontogenic diseases.
Postural Abnormality Chain Reactions
The proliferation of electronic devices has led to the phenomenon of \tech neck\—for every 15-degree increase in the forward angle of the cervical spine, the load on the neck doubles. Physical therapists recommend a wall test to assess posture: when the heels, buttocks, and shoulder blades touch the wall, the back of the head should naturally contact the wall surface. If there is a significant gap, it indicates a forward cervical spine problem.
It is advisable to perform neck clock exercises every 45 minutes while working: imagine the tip of the nose as the hour hand and slowly draw circles with a diameter of 30 centimeters. Using an adjustable height standing desk can effectively alleviate cervicogenic headaches. The latest ergonomic research suggests that the center point of the screen should ideally be 15-20 degrees below eye level.
Symptom Recognition Guide
Typical Accompanying Symptoms
Patients with occipital neuralgia experience an electric shock-like pain when turning the neck, while tension-type headaches manifest as a tightening pressure. Clinical findings show that about 38% of patients mistakenly treat cervicogenic headaches as regular migraines. The key differentiating point is whether there is accompanying tenderness at the inner edge of the scapula.
Warning Neurological Signs
Sudden onset of double vision or visual field loss requires high vigilance. The American Stroke Association suggests the FAST recognition method: Face asymmetry (Face), Arm weakness (Arm), Slurred speech (Speech), Timely medical attention (Time). Especially if accompanied by projectile vomiting, there may be a risk of increased intracranial pressure.
Somatization Symptoms Association
Patients with vestibular migraines often report a sensation of imbalance akin to seasickness, with this dizziness potentially appearing up to 72 hours before a headache attack. Gastroenterologists remind that long-term use of NSAIDs for pain relief may lead to medication overuse headaches, accompanied by gastric burning and other gastrointestinal symptoms.
Psychological Dimension Impact
The incidence of depression among chronic headache patients is four times that of the general population. Cognitive neuroscientists have found that persistent pain alters the functioning of the prefrontal cortex, leading to decreased decision-making ability. It is recommended to maintain a pain-emotion diary, simultaneously recording physiological sensations and psychological states, which can help formulate personalized treatment plans.
Timing for Medical Intervention Assessment
Observation of Disease Course Evolution
If the headache pattern changes—for example, increasing from twice a month to three times a week, or the nature of pain shifting from dull to sharp, this may signal disease progression. Neurologists pay special attention to three new aspects: newly onset headaches, new types of headaches, and new accompanying symptoms.
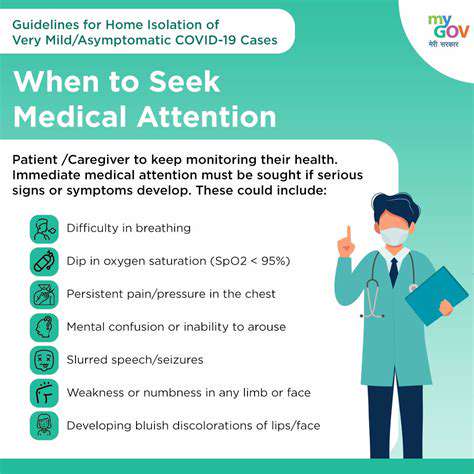
Identification of Dangerous Signs
A thunderclap headache (reaching maximum intensity instantly) requires immediate medical attention, as this may indicate a subarachnoid hemorrhage. Emergency department data shows that 25% of such patients have delayed diagnosis by taking painkillers before seeking medical help. Remember: severe headaches that acetaminophen cannot relieve are always worth monitoring.
Drug Interactions
Patients on anticoagulant medications who develop new headaches need immediate monitoring of coagulation indicators. Certain antibiotics (such as metronidazole) may cause severe headaches when combined with alcohol, and pharmacists remind that alcohol should be strictly avoided during medication use.
Self-Care Strategies
Non-Pharmacological Relief Measures
Applying peppermint essential oil to the temples can create a cooling effect, alleviating pain by activating TRPM8 receptors. Japanese researchers found that applying a cooled wet towel (to 13°C) to the carotid sinus area (below the angle of the jaw) can reduce headache intensity by two levels within five minutes.
Stepwise Medication Principles
The World Headache Society recommends a three-step therapy: first attempt magnesium supplementation (400mg/day), if ineffective, use triptans; in persistent cases, consider Botox injections. Note that taking pain relievers more than 15 days a month may lead to medication-rebound headaches.