Understanding the FODMAP Diet
The FODMAP protocol represents a specialized dietary approach for managing irritable bowel syndrome symptoms. This nutritional strategy involves restricting specific fermentable carbohydrates known to provoke digestive distress in sensitive individuals. By systematically eliminating then carefully reintroducing these compounds, individuals can identify personal triggers while allowing the digestive system to recover.
Comprehensive knowledge of FODMAP categories - including fructose, lactose, fructans, galactans, and polyols - forms the foundation for successful dietary management. This understanding enables informed food choices tailored to individual tolerance levels and symptom patterns.
Planning Your Elimination Phase
The initial elimination phase requires strict avoidance of high-FODMAP foods, necessitating thorough meal planning and preparation. This stage proves challenging for many due to the significant dietary modifications required. A strong support network greatly enhances the likelihood of successful adherence during this critical period.
Developing detailed meal plans ensures nutritional adequacy while maintaining dietary compliance. These plans should incorporate diverse low-FODMAP options to support overall health while managing symptoms.
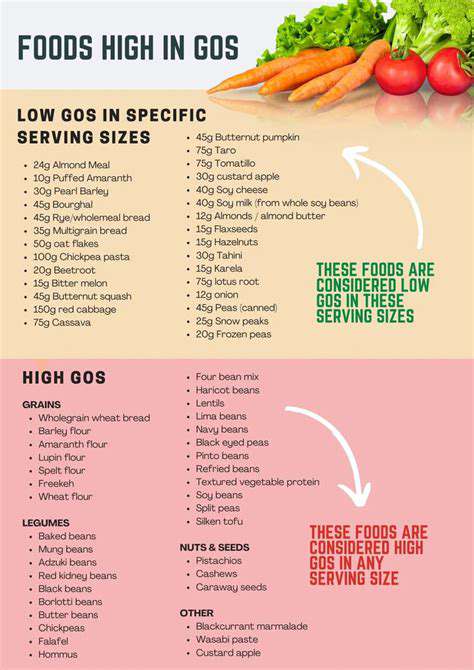
Identifying High-FODMAP Foods
Recognizing high-FODMAP ingredients demands careful scrutiny of food labels and composition. Many common fruits, vegetables, and dairy products contain substantial amounts of problematic carbohydrates, requiring thoughtful selection and substitution. Professional guidance from a registered dietitian often proves invaluable during this identification process.
Introducing Low-FODMAP Foods Gradually
The reintroduction phase involves methodical testing of individual FODMAP groups to determine personal tolerance thresholds. This process requires patience and careful symptom monitoring to accurately assess dietary responses.
Gradual reintroduction provides critical insights into individual digestive tolerances, enabling personalized long-term dietary adjustments. Detailed symptom tracking during this phase facilitates informed decision-making about sustainable eating patterns.
Understanding Nutritional Considerations
The restrictive nature of the FODMAP diet necessitates careful attention to nutritional balance. Ensuring adequate intake of essential nutrients may require strategic food selection or targeted supplementation in some cases.
Professional nutritional guidance helps create balanced eating plans that meet individual health requirements while managing symptoms effectively. Dietitians can also recommend appropriate supplements when dietary restrictions create nutritional gaps.
Long-Term Management and Sustainability
Sustained FODMAP management requires ongoing adaptation and lifestyle integration. Developing effective stress management techniques proves particularly important, as emotional factors significantly influence digestive health. This long-term commitment benefits from flexibility and continued support.
Practical strategies for social dining and travel help maintain dietary compliance in various settings. Educating friends and family about dietary needs facilitates social inclusion while managing health requirements.
Tracking Symptoms and Identifying Migraine Triggers
Understanding Migraine Symptoms
Migraine episodes present with diverse symptoms, making accurate self-assessment essential for effective management. Characteristic features often include unilateral throbbing pain of moderate to severe intensity, frequently accompanied by nausea, photophobia, and phonophobia. Recognizing these distinctive symptoms helps differentiate migraines from other headache types and guides appropriate treatment decisions.
Maintaining a detailed headache diary that records attack timing, duration, intensity, and associated symptoms provides valuable data for identifying patterns and potential triggers. This documentation serves as a crucial tool for developing personalized management strategies.
Identifying Potential FODMAP-Related Triggers
The FODMAP dietary approach may influence migraine frequency and severity for some individuals. As different FODMAP types affect individuals variably, careful observation of personal responses to specific food groups becomes essential. Methodical elimination and reintroduction of potential triggers, conducted under professional supervision, offers the most reliable approach for identifying dietary influences on migraine patterns.
Managing Migraine Triggers Through Dietary Modifications
Strategic reduction of high-FODMAP foods may decrease migraine frequency for certain individuals. This process requires careful implementation to maintain nutritional adequacy while testing dietary effects. Professional guidance ensures safe and effective dietary modifications tailored to individual health needs and migraine patterns.
Beyond the FODMAP Diet: Other Lifestyle Considerations
Beyond the FODMAP Diet: Exploring Underlying Issues
While effective for symptom management, the FODMAP approach often represents one component of a comprehensive treatment plan. Addressing potential emotional contributors like stress and anxiety frequently enhances treatment outcomes. The gut-brain axis plays a pivotal role in many digestive disorders, warranting consideration of psychological factors in addition to dietary modifications.
The FODMAP diet typically serves as an initial intervention rather than a permanent solution. Identifying and addressing root causes often yields more sustainable improvements than symptom management alone.
Lifestyle Factors and Gut Health
Holistic lifestyle approaches significantly influence digestive wellbeing beyond dietary considerations. Regular physical activity, quality sleep, and effective stress reduction techniques all contribute to maintaining a balanced gut environment. Incorporating mindfulness practices like meditation can further support digestive health by modulating stress responses.
The Importance of Mental Wellness
The bidirectional relationship between emotional state and digestive function underscores the importance of addressing psychological wellbeing in IBS management. Therapeutic interventions and stress management techniques often provide meaningful improvements in both digestive symptoms and overall quality of life.
Nutritional Supplements and Gut Health
Targeted nutritional supplementation may support gut health in some cases, though professional guidance ensures appropriate use. Prebiotics and probiotics represent common interventions, but individual needs vary significantly based on specific health circumstances.
Evidence-based supplementation can complement dietary strategies when implemented as part of a comprehensive care plan. Professional oversight prevents inappropriate or excessive supplement use.
Hydration and Gut Function
Adequate fluid intake supports multiple aspects of digestive function, from stool consistency to nutrient absorption. Maintaining proper hydration represents a simple yet frequently overlooked component of digestive health maintenance.
The Role of Professional Guidance
Effective management of digestive disorders typically requires multidisciplinary care. Collaboration with qualified healthcare providers ensures comprehensive evaluation and personalized treatment planning. This professional support proves invaluable for navigating the complexities of chronic digestive conditions and achieving optimal long-term outcomes.